Abstract
Backgrounds: Autologous stem cell transplant (ASCT) has been the standard treatment approach for patients with relapsed or high-risk lymphoma for several decades. Despite the improvement in supportive care, age has remained one of the critical factors that determines transplant eligibility and outcomes. Herein, we explored the transplant-related outcomes of patients with lymphoma aged 70 years or older at our institution and compared to those with younger ages.
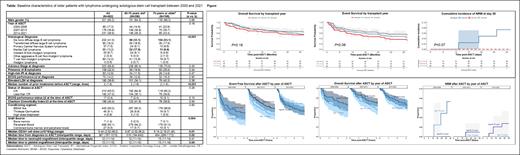
Methods: In this retrospective single center study, we include all patients with diagnosis of lymphoma who underwent ASCT between January 2000 and February 2021 at Mayo Clinic, Rochester, Minnesota. In addition to data obtained from the transplant database, we abstracted data from electronic medical record. We described relevant clinical characteristics and transplant associated outcomes including engraftment, transplant related mortality, relapse incidence, and survival outcomes. We compared the key transplant related outcomes with patients at the younger age group between 65 and 70 years old.
Results: A total of 196 patients with lymphoma aged 70 years or older underwent ASCT between January 2000 and February 2021. The median age of patients at the time of ASCT was 72.4 (70.0-78.7) years with 24 patients (12.2%) being older than 75 years old. Of 196 patients, 76 (38.8%) had Charlson comorbidity index of 3 or higher and 10 (5.1%) had performance status of 2 or higher at the time of ASCT. Table 1 summarizes the relevant baseline clinical characteristics of 196 patients in this cohort including the comparison with younger patients (age 65-70 years old, n=296). The most common transplant indication in this cohort was relapsed diffuse large B cell lymphoma. The majority of patients (91.3%) received peripheral blood graft with a median CD34+ cell dose of 5.14x10 6 cells/kg which was significantly lower than younger patients (P=0.01). The rate of neutrophil and platelet engraftment was 99.0% and 98.8% with corresponding median time to engraftment of 13 days for both cell lineages. The 30- and 100-day non-relapse mortality (NRM) of the entire cohort was 1.5% (95%CI 0-3.2%) and 4.6% (95%CI 1.6-7.5%) not statistically different between 70-75 years old and 75 years or older cohorts. With the median follow-up duration of 48 months, the 2-year event free survival (EFS) and overall survival (OS) was 55.9% (95%CI 49.2-63.5%) and 67.4% (95%CI 61.0-74.5%), respectively. Patients from the 70 years old or older cohort had similar EFS but inferior OS compared to the 65-70 years old cohort. However, there was no difference in EFS and OS between 70-75 and >75 years old cohorts. There was overall an improved trend of 30-day NRM, 2-year EFS and 2-year OS over the 3 different transplant periods (Figures). Although not statistically significant, patients who underwent ASCT between 2000 and 2006 had a trend towards higher 30-day NRM compared to patients who were transplanted at later time points (7.3% vs 0%, P=0.06). The major causes of death included progressive lymphoma, infection, and conditioning regimen related organ toxicities.
Conclusion: Outcomes of ASCT in older patients with lymphoma have improved over time with an excellent 30-day NRM (0%) in the past recent years. The major cause of treatment failure after ASCT was progressive disease. With appropriate patient selection, ASCT in older patients is feasible and provides acceptable outcomes comparable to the patients from younger age group.
Paludo: Karyopharm: Research Funding. Ansell: Bristol Myers Squibb, ADC Therapeutics, Seattle Genetics, Regeneron, Affimed, AI Therapeutics, Pfizer, Trillium and Takeda: Research Funding.