Abstract
Background: Early palliative care (PC) encounter has been shown to improve the quality of end-of-life (EOL) care. There is a significant increased in the PC utility of leukemia patients in the past decade. We aim to investigate the use of PC service in hospitalized patients with leukemia and other malignancies at the end of their life.
Methods: This is a retrospective study of National Inpatient Sample (NIS) with data year 2016-2018. The cohort of interest was adult patients (age at least 18) who had been hospitalized for at least three days and passed away. International Classification of Diseases, 10th Revision was used to identify patients with leukemia (myeloid, lymphoid and other types), other malignancies, comorbidities, PC encounters, and procedures. Primary outcome was PC encounter. PC-associated factors were analyzed with multivariate logistic regression. Statistical analysis was performed with SAS and R.
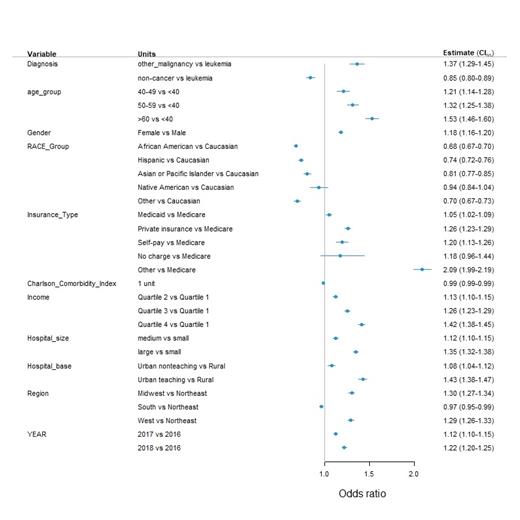
Results: Among 404,011 hospitalized patients who passed away, a total of 254,431 patients stayed in the hospital for at least three days. There were 5,819 (lymphoid: 2,177; myeloid: 2,848; other: 794) and 56,270 patients had leukemia and other malignancies, respectively. 51.4% leukemia, 57.4% other malignancies and 46.2% non-cancer patients had PC encounter. The PC use significantly increased in all subgroups from 2016 to 2018 (p < 0.0001). The PC utility of leukemia patients improved from 47.4% in 2016 to 55.4% in 2018. Compared to patients with other malignancies, leukemia patients had higher portion of mechanical ventilation use and cardiopulmonary resuscitation (CPR) prior to their death (31.6% vs 40.0%, p < 0.005). The PC utility was significantly higher in other malignancies group (adjusted odds ratio [aOR]: 1.37, p < 0.0001) and lower in non-cancer group (aOR: 0.85, p < 0.0001). Advanced age, female, Medicaid, private insurance, self-pay, higher income, larger hospital size, urban hospital, Midwest and West Region year of 2017 and 2018 were also associated with increased PC utility and African American, Hispanic, Asian or Pacific Islander, South region were associated with lower odds of receiving PC (Figure 1). Among leukemia patients, myeloid leukemia group had higher odds of PC encounter than lymphoid group (aOR: 1.28, p < 0.0001). African American, Hispanic, lower income, and smaller hospital were associated with significantly lower PC consult in leukemia patients.
Conclusion: There was an encouraging trend of increased PC consult between 2016 to 2018. Nevertheless, the PC utility was still lower among EOL hospitalized patients with leukemia than with other malignancies. Racial, socioeconomic, and hospital resource disparities were significant limiting factors of PC accessibility. Further systemic intervention and investigation are required to improve the disparities of PC utilization in leukemia patients.
No relevant conflicts of interest to declare.