Abstract
Extensive research has led to recent approval of novel therapies such as mylotarg, venetoclax, glasdegib and CC486, and small molecule inhibitors against actionable mutations such as ivosidenib (IDH1), enasidenib (IDH2), gliteritinib and midostaurin (FLT3) in AML. However, the mainstay of treatment in AML remains unchanged since the 1970s. There is a significant unmet need for AML patients that fail to respond to or relapse after standard-of-care (SOC) treatments including allogeneic stem cell transplantation and targeting actionable mutations. In addition, a large fraction of SOC patients invariably relapse due to persistence of chemotherapy-resistant leukemia stem cells (LSCs) or immune evasion. Therefore, identification of unique therapies that preferentially target elusive LSCs and promote immune responses to AML to prevent relapse are highly sought after. Unlike, targeting acute lymphoblastic leukemia (ALL) with CD19 or CD22 with various modalities, when developing AML therapies, it is of paramount importance to differentiate LSCs from hematopoietic stem cells (HSCs) to lessen or abolish unavoidable cytopenias.
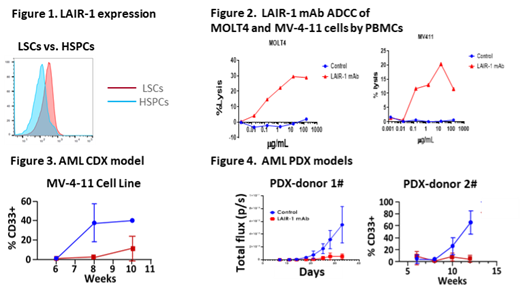
Leukocyte-associated immunoglobulin-like receptor 1 (LAIR-1) is an immune checkpoint receptor on T cells and myeloid cells that delimits immune cell activation through binding to endogenous collagen ligands. In addition, LAIR-1 is universally expressed on AML blasts and may sustain AML survival signals. We demonstrated using multi-color flow cytometry that LAIR-1 is highly expressed in AML blasts (n=9 of 9) and that LAIR-1 expression in LSCs (markers: CD34 +CD38 -CD90 -CD45RA +/- or CD34 -CD117 +CD244 +/-) is high compared with negligible expression of LAIR-1 in HSCs (markers: CD34 +CD38 -CD90 +CD99 -) (n=3) (Figure 1). Based on these findings, we hypothesized that a LAIR-1 monoclonal antibody (mAb) would disrupt LAIR-1 mediated survival signaling and preferentially target LAIR-1 expressing AML LSCs and blast cells but not HSCs. To test this, we developed a novel LAIR-1 targeting mAb with a functional human IgG 1 isotype that blocks LAIR-1 binding to its ligands (including collagens, complement component C1q, MBL and SP-D)
To characterize the anti-leukemic effect of the LAIR-1 mAb we performed an in vitro antibody dependent cell cytotoxicity (ADCC) assay with LAIR-1 expressing AML cells (MOLT4 and MV-4-11). Compared with isotype control, the LAIR-1 mAb significantly increased leukemia cell death (MV411 = 17% above isotype, and MOLT4 = 29.24% above isotype at 15 µg/ml), suggesting that the LAIR-1 mAb confers ADCC activity against LAIR1 + AML cells (Figure 2). To elucidate if the LAIR-1 mAb has a direct signaling effect on LAIR-1 + AML cells, a colony forming unit assay using primary AML cells was carried out. Interestingly, the LAIR-1 mAb inhibited colony formation by AML CD34 + cells (40-60% decreased compared with isotype control, N=4), but not normal CD34 + cells. These data suggests that our LAIR-1 mAb stimulated LAIR-1 signaling that inhibits LSC self-renewal. We then tested the in vivo anti-leukemia effect of the mAb in cell line derived xenograft (CDX) models (immune deficient mice transplanted with MV-4-11 expressing luciferase). In vivo bioluminescence imaging indicated that the LAIR-1 mAb significantly inhibited in vivo AML growth (91% reduction of total flux)(Figure 3). A significant increase in cell death was observed in the presence of the mAb in the blood (47%), spleen (89.4%) and bone marrow (27.6%). Similar to the anti-leukemic effect in CDX AML models, the LAIR-1 mAb significantly suppressed in vivo growth of AML patient derived xenografts (5 different primary AML donors) (10-90% human CD33 + AML cells in isotype control treatment vs 0.5-5% CD33 + AML cells in anti-LAIR-1 treatment, N=3) (Figure 4), while minimally impacting normal immune cells.
Taken together, our studies suggest that the LAIR-1 mAb we generated is a novel AML immunomedicine that preferentially eradicates AML LSCs and blasts while preserving healthy HSCs through disruption of AML survival signals and clearance of AML through ADCP and ADCC. Additional studies are currently evaluating if this novel LAIR-1 mAb has other mechanisms of action that contribute to overall in vivo activity, including reduction of AML niche implantation, regulation of bone marrow homing and regulation of anti-tumor immunity.
Tian: NextCure: Ended employment in the past 24 months. Paucarmayta: NextCure: Current Employment. Lovewell: NextCure: Current Employment. Maloveste: NextCure: Current Employment. Copeland: NextCure: Current Employment. O'Neill: NextCure: Current Employment. Patel: NextCure: Current Employment. Liu: NextCure: Current Employment, Current holder of stock options in a privately-held company. Myint: NextCure: Current Employment, Current holder of stock options in a privately-held company. Langermann: NextCure: Current Employment, Current holder of stock options in a privately-held company. Flies: NextCure: Current Employment, Current holder of stock options in a privately-held company. Kim: Nextcure: Research Funding.