Abstract
Background
Socioeconomic Status (SES) is recognized as a major contributor to health disparities in overall disease rate, morbidity, mortality, and quality of life (QOL). Specifically, low SES, independent of race, has a negative impact on solid and haematological cancer outcomes. Chimeric antigen receptor (CAR) T-cell cancer therapy is an increasingly utilized novel treatment option for the treatment of lymphoma; however its use is associated with cytokine release syndrome (CRS), neurotoxicity (NTX), and QOL impairments. Though the precise mechanism for these toxicities is unknown, adverse effects of CAR T-cell therapy are associated with neuroinflammatory markers that are upregulated in low SES populations. In this study, we hypothesized that patient response to a novel anti-CD20 and anti-CD19 (LV20.19) CAR T-cell treatment is affected by patient SES. Our second goal was to explore several possible biological mechanisms of the effects of SES on CAR T-cell therapy outcomes, including cytokines and kynurenine metabolites.
Methods
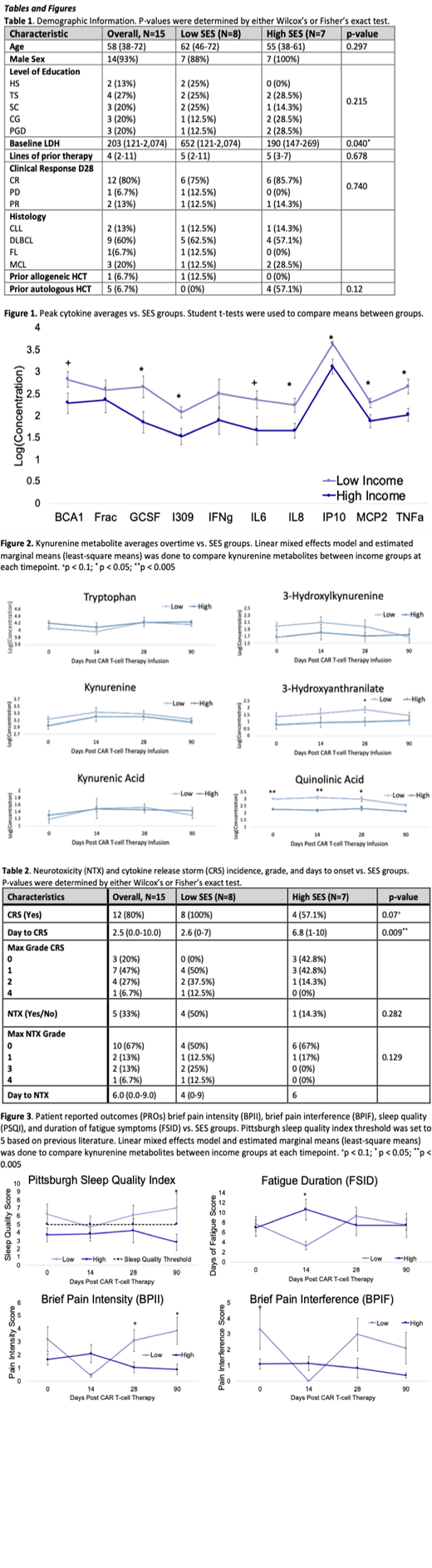
The current study population (N=15) is derived from a parent study evaluating patients treated with LV20.19 CAR T-cells on a Phase I/Ib clinical trial (NCT03019055). Patients provided blood samples and patient reported outcome (PRO) data 15 days before therapy (baseline), Day 14 post therapy (D14), D28, and D90. Cytokines were sent to Eve Technologies and quantified using an ELISA. Our analysis focused on 10 cytokines associated with CAR T-cell therapy neurotoxicity. Tryptophan (TRP) and kynurenine metabolites were quantified from serum samples using stable isotope-dilution liquid chromatography/mass spectrometry of the daughter ions (LC-MS-MS). Neurotoxicity was graded using the National Cancer Institute Common Terminology Criteria for Adverse Events v5 and CRS was graded using Lee et al. (Blood; 2019) PROs included depression and anxiety (Inventory of Depression and Anxiety), sleep (Pittsburgh Sleep Quality Index; PSQI), fatigue (Fatigue Symptom Inventory; FSI), and pain (Brief Pain Inventory; BPI) intensity (BPII) and interference (BPIF). SES was assessed by household annual income either above or below the Wisconsin median annual income in 2021 of $54,660 (high SES as >$55,000, n=7; low SES as $10,001-55,000, n=8). SES groups were compared against therapy outcomes using Wilcox Ranked Sum test, Student's t-test, and mixed effects linear models with a random subject intercept and estimated marginal means, respectively.
Results
There was no significant difference between SES groups based on age, education, or clinical response to therapy by D28 (Table 1). Baseline LDH was 3.4-fold higher in low compared to high SES patients (p=0.04). Most peak cytokine concentrations were higher in low SES patients with significant elevations (p<0.05) in G-CSF, I-309, IL-8, IP-10, MCP-2, and TNFa (9-fold, 3-fold, 3-fold, 2-fold, 2-fold, and 4-fold, respectively; Figure 1). Low SES patients also had significantly elevated neurotoxic pathway kyunerine metabolites (p<0.05; Figure 2) 3-hydroxyanthranilate (3-HAA) at D28 (8-fold) and quinolinic acid (QA) at baseline (5-fold), D14 (8-fold), and D28 (6-fold). Though incidences of CRS were only qualitatively higher in low SES patients (p=0.07), low SES patients experienced CRS significantly earlier (p=0.009; Table 2). Not enough patients experienced NTX for sufficient analysis. Patients with low SES indicated more pain intensity on D90 (BPII; p=0.021) and baseline pain interference (BPIF; p=0.08; Figure 3). Low SES patient reported worse sleep quality at D90 than high SES patients (p<0.05), and low SES average was higher than the PSQI threshold for "poor sleep" (5) at baseline, D28, and D90.
Conclusion
Our data show preliminary evidence that SES is associated with biological and clinical outcomes among patients receiving CAR T-cell therapy. In particular, we observed significantly higher concentrations of proinflammatory cytokine and neurotoxic kynurenine metabolites in low SES patients, as well as higher baseline LDH associated with higher tumor burden. Earlier CRS onset and increased pain were also seen in low SES patients, with qualitatively higher incidences of CRS, neurotoxicity, and poor sleep. Future work will focus on acquiring a larger sample to further delineate the impact of SES on cancer outcome disparities among CAR T-cell recipients, including but not limited to PROs, neurotoxicity, and survival.
Shah: Umoja: Consultancy; Incyte: Consultancy; Kite: Consultancy; Epizyme: Consultancy; Miltenyi Biotec: Consultancy, Honoraria, Research Funding; Legend: Consultancy; Lily: Consultancy, Honoraria, Research Funding. Hillard: Formulate Bioscience: Current holder of stock options in a privately-held company; Phytecs, Inc.: Membership on an entity's Board of Directors or advisory committees, Research Funding.