Abstract
Introduction: Allogeneic stem cell transplantation (HSCT) offers still the best chance for relapse-free long-term survival for most patients (pts) with acute myeloid leukemia (AML). Allogeneic HSCT may be performed as first line consolidation or following first relapse. Evaluation of measurable residual disease (MRD) at the time of HSCT allows for risk stratification apart from genetic risk at diagnosis. Outcomes of pts transplanted in first vs. second complete remission (CR) or CR with incomplete recovery (CRi) have not been assessed in the context of MRD status at HSCT.
Methods: We analyzed 580 AML pts consolidated by allogeneic peripheral blood HSCT at a median age of 60 (range 16-77) years in either first (79%) or second (21%) complete remission (CR) or CR with incomplete peripheral recovery (CRi). Conditioning regimens were non-myeloablative (66%), reduced-intensity (6%) or myeloablative (28%) according to EBMT guidelines. At diagnosis, cytogenetics, and the mutation status of CEBPA, NPM1 and presence of FLT3-ITD were assessed. Using a next-generation targeted amplicon sequencing approach we analyzed a panel comprising 54 recurrently mutated genes in myeloid malignancies on the MiSeq platform (Illumina). In pts with adequate material available (n=300), MRD status at HSCT based on NPM1 mutations , BAALC, MN1, and WT1 expression were evaluated and interpreted as published previously (Lange 2010, Jentzsch 2017 & 2019, Bill 2018). MRD pos pts were defined by being positive for any of the analyzed markers. Median follow up after HSCT was 3.9years.
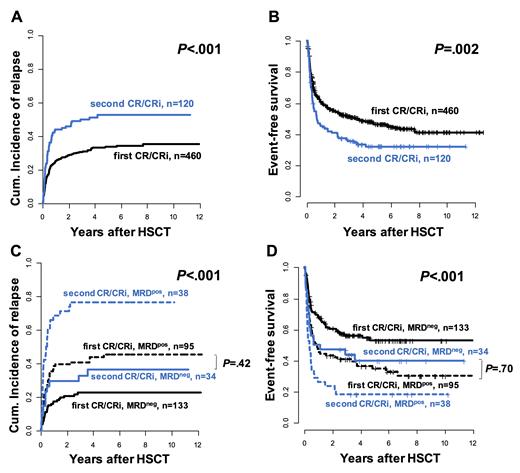
Results: Compared to pts transplanted in first CR/CRi, pts in second CR/CRi were less likely to have a secondary AML (P=.002). They less frequently had a monosomal (P<.002) or complex (P<.001) karyotype, but were more likely to have a normal karyotype (P<.001), to be NPM1 mutated (P=.001), to be biallelic CEBPA mutated by trend (P=.09), and to harbor a FLT3-ITD (P=.04). Pts in second CR/CRi received significantly less chemotherapy prior to HSCT (relapse to HSCT, 71%, 26%, and 3% of pts received 1, 2, or 3 or more cycles, respectively) than pts in first CR/CRi (diagnosis to HSCT, 16%, 61%, and 23% of pts received 1, 2, or 3 or more cycles, respectively, P<.001). Pts transplanted in second CR/CRi tended to more often be MRD pos (P=.10) and had a significantly higher cumulative incidence of relapse (CIR, P<.001, Figure 1A) and significantly shorter event-free survival (EFS, P=.002, Figure 1B) than pts transplanted in first CR/CRi. The MRD status at HSCT was an important prognostic factor in both pts transplanted in first (CIR, P<.001 and EFS, P=.002) and second CR/CRi (CIR, P<.001 and EFS, P=.04, Figure 1C,D). Similar results were obtained when we analyzed the four MRD markers separately. Noteworthy, MRD pos pts transplanted in first CR/CRi and MRD neg pts transplanted in second CR/CRi had similar CIR (P=.42) and EFS (P=.70), which again reflects the worse outcomes of AML pts transplanted in second compared to first CR/CRi as well as the prognostic significance of MRD assessment irrespective of the adapted markers.
In the clinically highly relevant group of ELN intermediate risk AML pts where the optimal consolidation (chemotherapy vs. allogeneic HSCT) remains a matter of debate, both MRD neg pts transplanted in in first or second CR/CRi had favorable outcomes (at three years, CIR 15% and 13%, respectively, and EFS, 64% and 63%, respectively), while outcomes were intermediate in MRD pos pts transplanted in first CR/CRi (at 3 years, CIR 38%, and EFS 46%) and very dismal in MRD pos pts transplanted in second CR/CRi (at 3 years, CIR 86%, and EFS 14%).
Conclusion: Despite pts transplanted in second CR/CRi had better disease risk at diagnosis, including a lower incidence of monosomal or complex karyotypes, secondary AML and a higher incidence of NPM1 mutations, they had a higher CIR and shorter OS than pts transplanted in first CR/CRi. While the MRD status at HSCT remained an important risk factor independently of the number of remission, MRD pos pts transplanted in first CR/CRi had comparable outcomes as MRD neg pts transplanted in second CR/CRi. The adverse outcomes of MRD pos patients and pts transplanted in second CR/CRi should be taken into account when planning consolidation treatment in AML pts. Benefit of additional therapies prior to HSCT should be evaluated to improve outcomes of eligible MRD pos AML pts, especially when transplanted in second CR/CRi.
Jentzsch: Astellas: Honoraria; Jazz Pharmaceuticals: Honoraria; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees. Backhaus: Bayer: Other: Current Employment of Family Member. Franke: Novartis: Honoraria; MSD: Honoraria; Jazz Pharmaceuticals: Honoraria, Other: Travel Sponsoring; Gilead: Honoraria, Other: Travel Sponsoring; BMS: Honoraria; Pfizer: Honoraria. Vucinic: Novartis: Honoraria; Janssen: Honoraria, Other: Travel Sponsoring; Abbvie: Honoraria, Other: Travel Sponsoring; Gilead: Honoraria, Other: Travel Sponsoring; MSD: Honoraria. Platzbecker: Geron: Honoraria; Novartis: Honoraria; Takeda: Honoraria; AbbVie: Honoraria; Janssen: Honoraria; Celgene/BMS: Honoraria. Schwind: Novartis: Honoraria, Research Funding; Pfizer: Honoraria.