Abstract
Background: The relationship between venous thromboembolism (VTE) and lymphoma is well established. In recent years, direct oral anticoagulants (DOACs) have been adopted as a treatment option for cancer associated thrombosis, however the majority of data using DOACs is in solid tumor patients. Here, we report the risk of recurrent VTE, bleeding outcomes, and effect of VTE on survival among lymphoma patients treated in a large centralized cancer associated thrombosis clinic.
Methods: We prospectively followed lymphoma patients referred to our clinic from 8/2014-01/2021. VTE events including deep venous thrombosis (DVT), pulmonary embolism (PE), and visceral vein thrombosis (VVT), were noted. Overall survival (OS) was estimated by Kaplan-Meier and compared using log rank test. Cumulative incidence rate of VTE was estimated and compared using Gray's method.
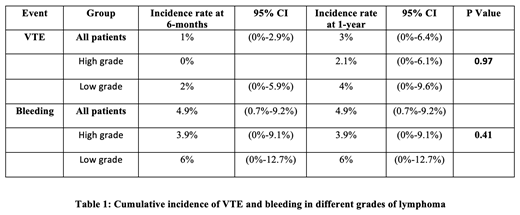
Results: A total of 103 patients were referred to our clinic due to clinical suspicion of VTE, of whom 40 (38.8%) were diagnosed with an acute VTE. The median age of the study population was66 (range 19-88), 61.2% were male and 16.5% had prior VTE. Non-Hodgkin Lymphoma (NHL) compromised 87.4%, with diffuse large b-cell lymphoma (DLBCL) being the most common subtype. Most patients had stage 4 disease (55.34%), had high grade lymphoma (defined as grade 3-4) (51.46%), and were on antineoplastic treatment (71.67%) at the time of VTE diagnosis. Site of VTE was DVT in 35.9%, PE in 5.8%, both DVT and PE in 2.9% and VVT in 0.97% of patients. Of these, 21 (20.39%) received a (DOAC), 14(13.59%) received enoxaparin, and 2(1.94) had IVC filter placed due to contraindication to anticoagulation. VTE recurrence occurred in 10% patients (total n=4; 2 were on enoxaparin and 2 were on rivaroxaban). Cumulative incidence of VTE in all patients at 6 months was 1% (95% CI: 0-2.9%), at 1 year was 3% (95% CI: 0-6.4%) with no significant difference in VTE or bleeding rates between lymphoma types or grade groups (P >0.05) (Table 1). Of 37 patients on anticoagulation, 10.8% experienced bleeding events (n=4) , of which 1 (2.7%) had major bleeding on IVC filter and 3 (8.1%) had CRNMB (2 on enoxaparin and 1 on rivaroxaban) at 6 month follow-up. Median follow-up was 35.9 months (range: 0.4-77.7 months) and median 2 year OS was 76%, 95% CI (68-85%). Overall survival was negatively impacted by age (patients over age 65 had a 2 year OS rate of 67%95% CI (0.56-0.81), p=0.01). Lymphoma grade had no impact on OS (2-year OS rate= 0.69, 95% CI (0.57-0.84), P=0.1132)
Conclusion: High grade and low grade lymphoma patients treated in our centralized cancer thrombosis clinic had a 10% chance of VTE recurrence when treated with DOAC or enoxaparin. Bleeding rates were low in both groups; however, we saw decreased overall survival in those treated with DOACs. This data adds to the growing knowledge of treating hematologic malignancies with direct oral anticoagulants, but larger studies are needed to study the safety and efficacy of these agents in lymphoma patients.
Khorana: Halozyme: Consultancy, Honoraria; Anthos: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria; Sanofi: Consultancy, Honoraria; Bristol Myers Squibb: Consultancy, Honoraria; Janssen: Consultancy, Honoraria; Bayer: Consultancy, Honoraria. Angelini: Sanofi: Membership on an entity's Board of Directors or advisory committees.