Abstract
In October 2021, brexucabtagene autoleucel became the first anti-CD19 chimeric antigen receptor T-cell product to receive approval from the Food and Drug Administration to treat adults with relapsed and refractory B-cell acute lymphoblastic leukemia. The approval is based on results from the Zuma-3 trial and significantly widens treatment options for this patient population. In this article, we review outcomes from this study and its implications.
Introduction
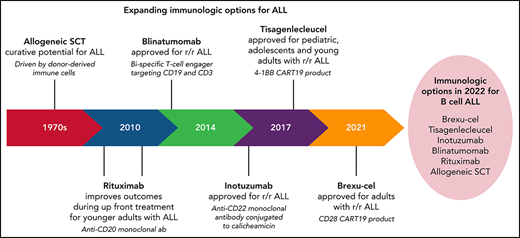
Chimeric antigen receptor T-cell therapies targeting CD19 (CART19) have transformed the treatment paradigm for patients with relapsed and refractory (r/r) B-cell malignancies. Commercial CAR T-cell products to date have included either a CD28 or a 4-1BB costimulatory domain, which correlates with distinctive cellular kinetic patterns, the potential impact of which is still evolving and is discussed below. The first drug in this class to receive an indication by the Food and Drug Administration was tisagenlecleucel, a CART19 product bearing a 4-1BB costimulatory domain that was initially approved for pediatric and young adult patients up to the age of 25 with acute lymphocytic leukemia (ALL) that was refractory or in second or greater relapse.1,2 Since then, varied CART19 products, including tisagenlecleucel, axicabtagene ciloleucel, lisocabtagene maraleucel, and axicabtagene autoleucel, have been approved for different subsets of patients with r/r non-Hodgkin lymphoma, but an indication for adults over the age of 25 with r/r ALL has been lacking.3-6 This has been in part due to a differential tolerability of CART19’s severe treatment-related toxicities of cytokine release syndrome (CRS) and immune effector cell–associated neurotoxicity syndrome (ICANS) in adults with ALL compared with their pediatric cohorts. An early multisite clinical trial for adults with r/r ALL treated with JCAR 015, a CART19 with a CD28 costimulatory domain, was closed after treatment-related deaths from cerebral edema.7 Toxicity observations in other trials in ALL utilizing both 4-1BB and CD28 containing CARTs led to delays to allow for modifications in clinical trial design to improve safety.
With optimization, various CART19 products with CD28 or 4-1BB costimulatory domains have been shown to be effective in single-center studies for adults with r/r ALL. Across these trials, remissions for adults with r/r ALL ranged from 69% to 85% and were mostly measurable residual disease (MRD) negative by 1-month postinfusion. Remissions were not discriminated by number and type of prior therapy, disease mutational status, or history of prior allogeneic hematopoietic stem cell transplantation (HSCT) (Table 1).8-10 Interestingly, in some trials, CART19 cells have been observed in the cerebral spinal fluid, offering antileukemic protection in this space.11-13 Median overall survival (mOS) beyond 1 year is seen across most CART19 studies in ALL and importantly is noted within some reports to vary by dose level or other modifications made throughout the trial. Recently, results from larger multicenter studies in adults with r/r ALL have been reported, providing more generalizable outcomes.14-16 One of these trials is Zuma-3, the results of which led to the approval of brexucabtagene autoleucel (brexu-cel, Tecartus) for adults with r/r ALL, allowing for the first-time commercial CART19 access for adults with r/r ALL over 25 years.
Brexu-cel in ALL: Zuma-3 and commercialization
Product overview
Brexu-cel is an autologous CART19 product containing a CD28 costimulatory domain that was originally approved to treat adults with r/r mantle cell lymphoma (MCL)5 and more recently approved to treat adult patients with r/r ALL. Of interest, dosing for patients with ALL (1 × 106 cells per kg) and the intensity of chemotherapy conditioning (fludarabine [25 mg/m2 on days −4, −3, −2] and cyclophosphamide [900 mg/m2 on day −2]) are lower than for the treatment of patients with MCL. Cell dose and extent of lymphodepletion are both modifiable factors that can impact the peak expansion of CART19 and resulting cytokine elevations and thus toxicity,17 and these modifications likely improved the safety profile for brexu-cel in r/r ALL. Although Brexu-cel consists of the same CAR construct as axicabtagene autoleucel, it differs in its manufacturing process, which removes malignant cells from the leukapheresis product in an effort to minimize early ex vivo activation and exhaustion of the CART19 cells.
Trial design and population treated
Zuma-3 is a multicenter, international phase 1 to 2 single-arm clinical trial (NCT02614066) to evaluate the safety and efficacy of KTE-X19 (brexu-cel) in patients over the age of 18 years with r/r B-cell ALL. The phase 1 portion of the study treated 45 patients and identified 1 × 106 cells per kg as the recommended dose for further study in phase 2.15 To be eligible for the phase 2 portion of the study, patients needed to have >5% morphologic bone marrow blasts with r/r disease that was either (1) primary refractory, (2) in first relapse with initial remission <12 months, (3) relapsed or refractory after 2 or more prior lines of therapy, or (4) relapsed after allogeneic stem cell transplant (HSCT). Prior blinatumomab was permitted if ≥90% of blasts were CD19+. Corticosteroids (>5 mg/d of prednisone or equivalent) and other immunosuppressive drugs were avoided for 7 days prior to leukapheresis. Patients were permitted to undergo bridging therapy to control disease while awaiting return of manufactured product after leukapheresis. Patients received conditioning chemotherapy with fludarabine (25 mg/m2 on days −4, −3, −2) and cyclophosphamide (900 mg/m2 on day −2) prior to CART19 infusion.16
A total of 71 patients were enrolled in the phase 2 portion and underwent leukapheresis at 25 sites across North America and Europe. Manufacturing was successful for 65 patients (92%), and 55 patients (77%) were infused. The median time from leukapheresis to release of product was 13 and 14.5 days for US and European patients, respectively. The median age for infused patients was 40 years, with 8 (15%) patients ≥65 years. Overall, the patients were heavily pretreated and representative of r/r patients in the modern era with 42% having received prior blinatumomab, 22% having received prior inotuzumab, and 45% relapsing after a prior HSCT. In addition, many patients had significant disease burden in the bone marrow, with 34 (62%) patients having >25% bone marrow blasts. Although some patients had a recent history of central nervous system (CNS) disease, all patients had CNS1 disease at baseline before starting conditioning chemotherapy. Fifteen patients (33%) had Philadelphia chromosome+ disease and were permitted to restart their tyrosine kinase inhibitor 2 months after infusion.
Toxicity
Per protocol, patients were monitored in an inpatient setting for at least 7 days after brexu-cel infusion. After 2 treatment-related deaths early in the phase 1 portion of Zuma-3, a revision was made to intervene earlier with corticosteroids for neurologic toxicity. Although overall more manageable, toxicity was still clinically significant in the phase 2 portion of the study. Disease burden in ALL has been strongly correlated with toxicity in CART19 trials, and the majority of patients in Zuma-3 had significant disease burden with >25% bone marrow blasts. The overall incidence of CRS in phase 2 was 89% with 24% of patients having grade 3 or 4 toxicity and 40% requiring vasopressors. The median time to onset of CRS was 5 (interquartile range [IQR] 3 to 7) days, and median duration was 7.5 (IQR 5 to 18) days. Overall, 60% of patients had neurologic toxicity with 25% having grade 3 events, and 1 patient had a grade 5 event owing to intracranial herniation. The median time to onset of neurotoxicity was 9 (IQR 7 to 11) days, and median duration was 7 (IQR 4 to 19) days. Most patients were treated with tocilizumab (80%) and/or corticosteroids (75%). Infections of grade 3 or greater occurred in 25% of patients, with 1 grade 5 event from sepsis.
Response and survival
The median follow-up for patients on the phase 2 portion of the study was 16.4 months. For infused patients, 39 (71%) patients achieved either complete remission (CR) or complete remission with incomplete hematologic recovery (CRi). For responders, 97% were minimal residual disease (MRD) negative by a flow cytometry assay with a sensitivity of 0.01%. Responses were not differentiated by patients aged >65 years or prior treatment with blinatumomab, inotuzumab, or HSCT. The mOS for the infused cohort was 18.2 months, and median relapse-free survival (RFS) both with and without censoring for HSCT was 11.6 months. mOS was not reached for those who achieved CR/Cri, and the median duration of remission (mDOR) for responders with and without censoring for HSCT was 12.8 months. DOR was defined as time from first CR to death or relapse. Disease assessments after HSCT were not used in derivation of DOR, but patients with Philadelphia chromosome+ disease who resumed tyrosine kinase inhibitors after achieving CR were included in the derivation of DOR. There were 10 patients (18%) who achieved CR/CRi and proceeded per physician discretion to HSCT.
Role of HSCT
Overview
For a patient with r/r ALL who achieves an MRD− CR after CART19 therapy, a key clinical question is whether to consolidate that remission with HSCT. There are no randomized studies to help guide this decision, and we have limited information from published single-arm studies that all use different CART19 products. As always when considering transplant, treatment-related morbidity and mortality need to be balanced against risk of relapse. Recipients of CART19 for ALL are at risk for both CD19+ and CD19− relapses, but the relative risks will vary by product and population treated, making it very challenging to extrapolate data regarding role of transplant from 1 trial to the next.
HSCT data from 4-1BB-CART19 including tisagenlecleucel
It is clear that a subset of patients with ALL treated with tisagenlecleucel and some other investigational CART19 products bearing a 4-1BB costimulatory have ongoing durable remissions without HSCT. These outcomes correlate strongly with the ability of CART19 to maintain functional persistence in vivo.1,8,9,14,18-20 Even when a particular 4-1BB–containing CART19 product has been shown to have good functional persistence however, that persistence is not observed across all patients treated, and CD19+ relapses (in addition to CD19− relapses from antigen escape) remain a significant challenge, which may be mitigated by HSCT in some patients.8,9
HSCT data from CD28-CART19 including brexu-cel
CAR T cells with CD28 costimulatory domains, including brexu-cel, have exhibited rapid early expansion without functional persistence beyond 3 to 6 months.5,15,16 It is less clear for these products if persistence is necessary for long-term RFS in patients with ALL that are not bridged to HSCT. The National Cancer Institute, for example, reported long-term outcomes for 50 children and young adults treated with a CD28-CART19 product, which contained the same CAR construct as brexu-cel, although with different manufacturing techniques. In this study, all patients who did not receive an HSCT relapsed at a median of 152 (range, 94 to 394) days.21 However, data from Memorial Sloan Kettering Cancer Center found that in 51 adults treated with a different CD28-CART19, no difference in outcomes was seen between those who did or did not proceed to HSCT.10 With brexu-cel, only 10 patients (18%) proceeded to HSCT on the phase 2 Zuma-3 trial, and the mDOR for the entire cohort was 12.8 months. As discussed in more detail above, DOR did not change with or without censoring for HSCT. The overall risks and benefits of HSCT after remission with brexu-cel will require longer follow-up and larger numbers of patients treated.
Brexu-cel vs other therapies
Outcomes in patients with r/r ALL treated with brexu-cel (CR = 71%; mOS = 18.2 months, mDOR = 12.8 months) compare favorably with those from patients treated with inotuzumab (INO-VATE study) (CR = 80.7%; mOS = 7.7 months; mDOR = 4.7 months) and blinatumomab (TOWER study) (CR = 35.1%; mOS=7.7 months, mDOR = 7.3 months), although these nonrandomized comparisons should be done with caution given differences in trial designs and patient populations.1,16,20,22,23 In addition, similar to many CART19 studies, the efficacy outcomes highlighted from Zuma-3 are for infused patients only. This discounts treatment failures from (1) lack of clinical window for leukapheresis, (2) manufacturing failure, and (3) inability to tolerate the treatment delay while awaiting manufacture. These are all factors that underscore the need for intent-to-treat outcomes to be measured.
Adult patients with chemotherapy refractory disease who have relapsed or failed treatment with inotuzumab and blinatumomab now have a highly effective salvage option with the commercial availability of brexu-cel. For patients with multiple options, choice of therapy will be based on an individual patient’s disease burden, therapeutic goals, prior treatment history, options for HSCT, anticipated toxicity from treatments available, and feasibility of brexu-cel. Feasibility issues for brexu-cel include availability of a treatment center, identifying clinical and logistical windows for leukapheresis and manufacture, and potential for patient stability while awaiting manufacture. Specific clinical factors may influence a clinician’s decision to treat with brexu-cel (Table 2). For a patient with low likelihood or desire to proceed to an HSCT if a CR is obtained, brexu-cel may be attractive owing to a relatively high anticipated mDOR (both with and without HSCT) of 12.8 months. A patient with a history of CNS disease may benefit from brexu-cel, as other CART19 products have been found in the cerebral spinal fluid of patients with ALL offering protection in this common sanctuary site that is not penetrable with most alternative systemic therapies.11-13 The anticipated toxicity from brexu-cel and its preceding conditioning chemotherapy need to be considered on an individualized basis to inform treatment decisions. Patients with high disease burden, advanced age, and comorbid cardiovascular disease, for example, may not tolerate anticipated severe CRS or ICANs, and another approach may be more appropriate. If the goal for the patient is clearly an HSCT if they achieve an MRD− CR, there is no evidence that brexu-cel vs an alternative approach improves RFS after HSCT.24,25
Conclusions
The commercial availability of brexu-cel represents a significant advancement in our ability to successfully care for adult patients with r/r ALL. The high incidence of CRS and ICANs underscores the need for individualized assessment of risk and the requirement for close patient observation. We now have the “luxury” of several immunotherapeutic approaches to treat relapsed disease, and further studies are needed to inform optimal timing and sequence of available interventions. Similarly, the role of HSCT after a CR from brexu-cel requires ongoing exploration, with limited data available currently to guide this decision. CAR T-cell therapy for ALL continues to expand with the ongoing development of additional products and targets along with better toxicity prevention and mitigating strategies.8,15,20,26-30
Authorship
Contribution: N.V.F. wrote the paper.
Conflict-of-interest disclosure: Novartis: Research Support; Kite Pharma: Consultancy; Sana Biotechnologies: Consultancy; Pfizer: Consultancy.
Correspondence: Noelle V. Frey, Hospital of the University of Pennsylvania, Abramson Cancer Center, Perelman Center for Advanced Medicine, 3400 Civic Center Blvd, Philadelphia, PA 19104; e-mail: Noelle.frey@pennmedicine.upenn.edu.