In this issue of Blood, Borogovac et al1 report a high frequency of patient-reported stroke, neurologic complications, and cognitive impairment in hereditary thrombotic thrombocytopenic purpura (hTTP, also called congenital TTP), including many strokes that preceded the diagnosis of hTTP. These results reinforce the need for universal, early, and effective prophylaxis in patients with hTTP to prevent both potentially devastating strokes and other hTTP complications. Greater awareness of stroke as a complication of hTTP is also required to prevent delayed diagnosis and subsequent hTTP morbidity.
hTTP is a rare form of TTP in which the severe ADAMTS13 deficiency is caused by inheritance of biallelic ADAMTS13 gene mutations instead of the far more common acquired immune-mediated form of TTP. Treatment for acute episodes of hTTP involves either plasma or plasma exchange (to prevent volume overload). The only prophylaxis options are either plasma transfusion on an every-2-weeks basis or plasma-derived factor VIII concentrates that are rich in ADAMTS13 (Koate-DVI or BPL 8Y), which pose a theoretical increased risk of thrombotic complications.2,3 The high burden of chronic transfusions and lack of recognition of the benefit of prophylaxis are currently major barriers to adequate prophylaxis in hTTP.
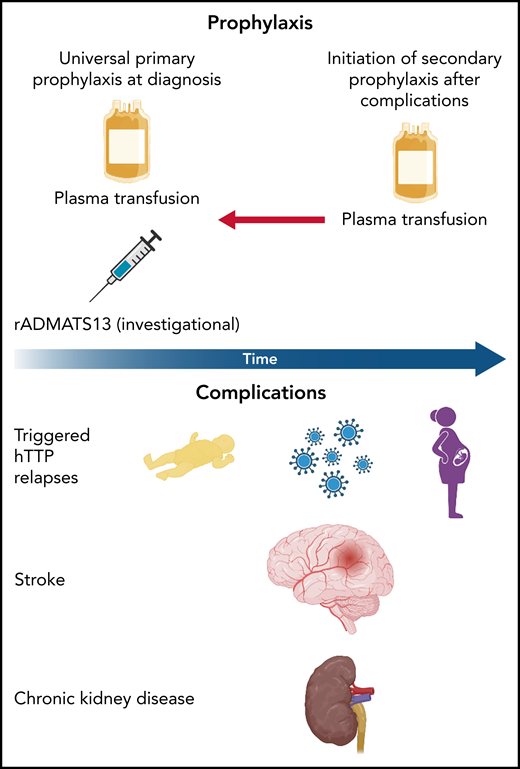
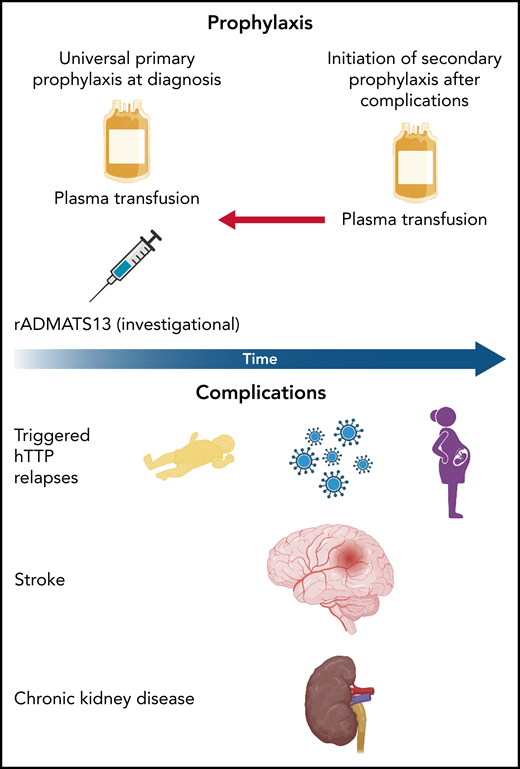
hTTP is challenging to diagnose and, even when identified, it is difficult to prevent complications such as premature stroke and transient ischemic attack (TIA), chronic kidney disease, and relapses of hTTP. The diagnosis is usually made during hTTP episodes that typically occur during infancy, pregnancy, or inflammation (most commonly, alcohol use in older patients and infection in children) (see figure). Obviously, many of the signs and symptoms are the same as seen in immune-mediated TTP (iTTP). Both have kidney injury, but acute kidney injury is typically mild in iTTP. In hTTP, kidney injury associated with hTTP relapses is severe, with previous reports from the International hTTP Registry finding that 12.5% of patients required hemodialysis or renal transplantation and 25% had chronic kidney disease.5 There is increasing evidence that stroke is a complication shared by both disorders. In iTTP, risk for stroke is associated with ADAMTS13 deficiency during remission.4 Premature stroke and TIA are established complications of hTTP, with nearly 30% of participants and more than half of participants over 40 years old reporting a major thromboembolic event to the International hTTP registry.5 A report from the UK TTP Registry found that >20% of participants with hTTP experienced stroke or TIA, with a much lower incidence among individuals on prophylaxis.6
Currently, prophylaxis with plasma transfusions is recommended in patients with hTTP and most frequently, although inconsistently, is initiated only after complications from the disease have arisen (upper panel). Given the high frequency of stroke and neurologic impairment reported by patients in Borogovac et al, the authors make a strong case for prophylaxis from the time of diagnosis. Complications of hTTP (lower panel) include hTTP relapses during the neonatal period associated with neonatal jaundice, infections (particularly childhood illness), and pregnancy along with stroke and chronic kidney disease. The authors highlight the fact that stroke often preceded the hTTP diagnosis, which suggests an important need to make this diagnosis early to prevent major neurologic morbidity. Illustration created using Biorender.
Currently, prophylaxis with plasma transfusions is recommended in patients with hTTP and most frequently, although inconsistently, is initiated only after complications from the disease have arisen (upper panel). Given the high frequency of stroke and neurologic impairment reported by patients in Borogovac et al, the authors make a strong case for prophylaxis from the time of diagnosis. Complications of hTTP (lower panel) include hTTP relapses during the neonatal period associated with neonatal jaundice, infections (particularly childhood illness), and pregnancy along with stroke and chronic kidney disease. The authors highlight the fact that stroke often preceded the hTTP diagnosis, which suggests an important need to make this diagnosis early to prevent major neurologic morbidity. Illustration created using Biorender.
In this issue of Blood, Borogovac et al further clarify the burden of neurologic complications in US participants in the International hTTP Registry through patient interviews, and the clarity is alarming. Borogovac and colleagues found nearly two-thirds of US participants in the registry reported being diagnosed with a stroke, with a median age in their twenties, and many had residual symptoms and/or recurrent strokes. Importantly, for many, the diagnosis of hTTP came many months or years after their stroke. None were on prophylactic treatment at the time of their stroke.
The much-heralded arrival of recombinant ADAMTS13 (rADAMTS13) for hTTP is likely to be an important new tool for prophylaxis and treatment of hTTP in much the same way that Factor VIII and IX concentrates changed the natural history of hemophilia.7 However, hTTP faces similar challenges: physicians must educate patients and parents on the benefits of prophylaxis to ensure adherence for adequate protection against both stroke and hTTP relapses. Likewise, vigilance for inhibitory ADAMTS13 antibodies is required. It is imperative to inform patients about the risks of stroke and neurological sequelae as key reasons to strongly consider prophylaxis from the time of diagnosis.
Addressing the other major problem of delayed diagnosis, the authors rightly suggest the need to screen patients with embolic stroke of undetermined source (formerly cryptogenic stroke) for hTTP, a test that could influence management far more than inherited thrombophilia evaluations that are commonly used during stroke evaluations.8 Is there an opportunity to further reduce the morbidity of hTTP with earlier diagnosis, ideally before significant morbidity from stroke or kidney injury?
The UK TTP Registry found delayed diagnosis in patients with unexplained obstetric complications or patients who were misdiagnosed with chronic immune thrombocytopenia or Evans syndrome.6 An improved awareness of hTTP and a low threshold for testing patients with unexplained thrombocytopenia and obstetric complications are required to uncover new hTTP diagnoses and prevent future complications. Finally, in light of the morbidity of this disease and emerging better prophylaxis options, should hTTP be a priority for developing a newborn screening test? At a minimum, lowering the threshold for testing ADAMTS13 activity in patients with unexplained stroke, unexplained obstetric complications, and/or thrombocytopenia is necessary to improve diagnosis and outcomes in hTTP, and once the diagnosis of hTTP is made, early and consistent prophylaxis should be implemented to prevent serious morbidity, which will hopefully be more convenient and effective with rADAMTS13.
Conflict-of-interest disclosure: M.M. has received honoraria from Sanofi-Genzyme.