Abstract
Background: The prognosis of patients with multiple myeloma (MM) has significantly improved with the advancement of highly effective therapies. High dose chemotherapy with an autologous hematopoietic stem cell transplant (ASCT) continues to be the standard of care for eligible patients with MM. While several factors affect survival following ASCT, the impact of social determinants of health, especially the local level social vulnerability, on survival in this patient population is not well documented. This study will use the CDC Social Vulnerability Index (SVI) to capture local levels of social vulnerability. Composed of 15 social factors, SVI is a constantly evolving measure of a community's ability to respond to hazardous events and helps public health officials identify populations in most need of support. SVI has traditionally been used for natural disaster outreach, but recently has been studied in cancer patients. These social factors are grouped into four related themes (socioeconomic status, household composition and disability, minority status and language, and housing type and transportation), which comprise a community's overall vulnerability ranking. The areas with higher levels of SVI are at a higher risk during public health emergencies.
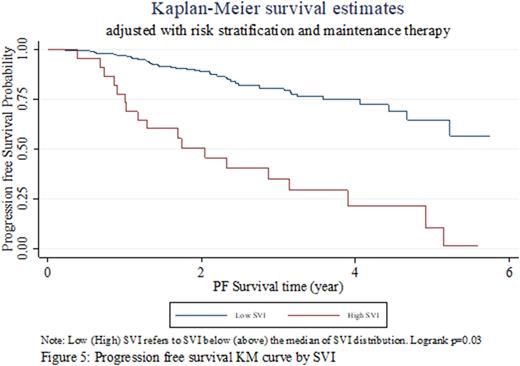
Aim: This study evaluated the impact of SVI and other social determinants of health on progression free survival (PFS) following an ASCT.
Methods: A retrospective analysis of patients who underwent an ASCT in a single center from 2012 to 2020 was conducted. Patients were followed from time of diagnosis to 5 years post-transplant, if applicable. Socioeconomic data was obtained using the transplant center's database, the 2003 rural-urban continuum codes provided by US Department of Agriculture, and the CDC SVI, which uses census statistical data to identify the most vulnerable populations. Variables examined included age, gender, race, primary insurance payor, geographic location (urban/rural), and SVI, with a higher SVI implying a greater level of vulnerability among the county. Logistic regression analysis was performed to determine the odds ratios (OR) for the primary endpoint of PFS and for the secondary endpoint of overall survival (OS), while controlling for characteristics. Logistic regression using both full set of control variables and stepwise selection method were used to identify key predictors of PFS and OS.
Results: 225 consecutive patients with MM who received ASCT participated, with the majority having been transplanted in the last 5 years. 151 (67%) achieved PFS at 5 years post-transplant and 171 (76%) remained alive at 5 years post-transplant. 209 (93%) patients received post-transplant maintenance therapy, and 77 (34%) had high-risk cytogenetics according to mSMART 3.0 criteria. The majority (72%) of the study population were Non-Hispanic White and most patients (60%) had public insurance payors. Race, insurance payor, or living in urban/rural areas did not affect PFS or OS. 53 (24%) patients lived in high SVI areas (SVI above median of SVI distribution). Treating SVI as a continuous value from 0 to 1, as the CDC scores SVI, we found that higher SVI values were significantly associated with lower odds of PFS post-transplant (OR=0.347, p<0.05). Patients living in higher SVI communities also saw a trend toward lower OS (OR=0.321) post-transplant (p<0.10). Of patients living in high SVI areas, only high-risk cytogenetics were significantly associated with lower odds of PFS (OR=0.0693, p<0.01) and OS (OR=0.294, p<0.05).
Conclusion: Data from this single center retrospective study demonstrated that a higher SVI was associated with a lower PFS, while race, insurance payor, and urban/rural location had no significant association with PFS. This suggests that areas with high SVI may need more resources to achieve optimal PFS. Future studies will focus on efforts to address the factors in SVI, so all patients have opportunities for excellent outcomes after ASCT for MM. Factors that may be prudent to concentrate on include transportation, housing, and employment, as these components may be more easily intervened upon in future studies.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.