Abstract
Background:
Previous studies have demonstrated the negative regulatory role of von Willebrand Factor (VWF) in angiogenesis involving extracellular and intracellular pathways that promote vascular endothelial growth factor (VEGF) signaling. These findings have provided direct evidence for the longstanding association between inherited and acquired abnormalities of VWF and the formation of angiodysplastic lesions, which continue to remain a major challenge. Understanding the role of VWF in angiogenesis could reveal new therapeutic targets that may lead to improved patient management strategies.
Aim: To examine the impact and mechanisms of localized VWF replacement on in vivo angiogenesis in a VWF-deficient mouse model.
Methods:
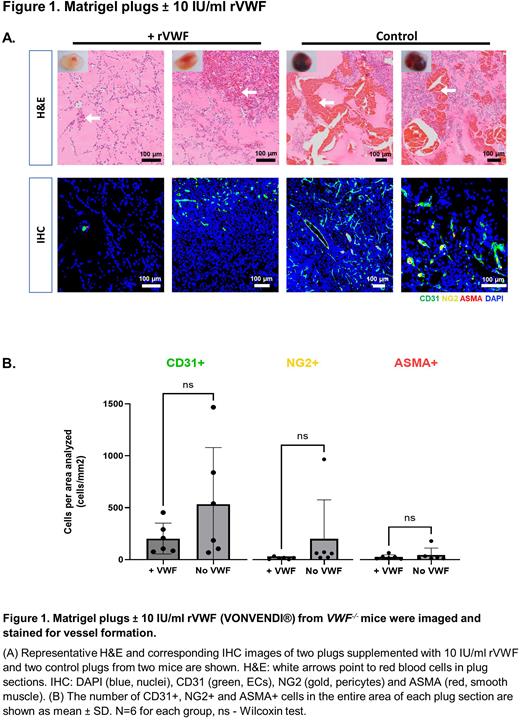
Three separate experiments were carried out in 10 to 12-week old C57Bl/6 VWF-/- mice of both sexes. In all experiments plugs were excised after seven days of incubation and processed for hematoxylin and eosin (H&E) and immunohistochemical staining (IHC) to assess vessel formation and vascular permeability/maturity, except for the directed in vivo angiogenesis assay (DIVAA) where there was technical difficulty in obtaining histological sections.
In the first experiment, DIVAA was employed to decrease inter-assay variability. Angioreactors containing Matrigel mixed with fibroblast growth factor (FGF), VEGF and varying doses of recombinant VWF (rVWF, VONVENDI®) were implanted subcutaneously in the right back flank of mice. Similar angioreactors without rVWF were implanted in the left back flank of mice as a control (N=15, 3 per dose group).
In the second experiment the in vivo Matrigel plug assay was used to enable histological evaluation of plugs. 300 μL of Matrigel mixed with FGF, VEGF and rVWF at 0.5IU/ml and 10.0IU/ml, was injected subcutaneously in the right back flank of each mouse based on dose group. In the left back flank, an equal volume of Matrigel without rVWF was injected as a control (N=12, 6 per dose group of rVWF).
The setup of the last experiment was similar to the second, however, Matrigel was supplemented with normal endothelial-colony-forming cells (ECFCs) as the source of localized VWF in place of rVWF, in a titration curve of cell numbers (1 x 105, 5 x 105, 1 x 106 cells; N=15, 3 per dose group).
Results:
Generally, there was a dose response gradient across all three experiments, with higher doses of rVWF or ECFC titres yielding more pronounced effects. In comparison to the lightly coloured angioreactors from the experimental group (supplemented with rVWF), those from the control group were dark red in colour indicating the presence of more vessels and erythrocytes in the Matrigel.
No clear differences were observed between plugs that received rVWF at 0.5 IU/ml and those that did not, both grossly and histologically. Most plugs with 10 IU/ml of rVWF appeared lighter in colour compared to those without rVWF. A similar pattern was observed on H&E staining with sections from plugs supplemented with rVWF showing fewer capillaries and red cells, compared with plugs that had only growth factors (Figure 1A). In line with these observations, IHC quantitation of endothelial cells (ECs), pericytes and smooth muscle cells showed a decrease in capillary formation and vessel maturity in rVWF supplemented plugs, although this did not reach significance (Figure 1B).
Compared to plugs that had ECFCs, those without ECFCs were dark red in colour, indicating the presence of more mature vessels with red cells. H&E staining of control plugs showed increased cellular infiltrate and capillary formation compared to those supplemented with ECFCs. Immunostaining of control Matrigel plugs also showed increased vascularization and maturity of vessels as evidenced by higher signals for neural/glial antigen 2 (NG2) stain for pericytes and alpha-smooth muscle actin (ASMA) which stains smooth muscle, compared to plugs with ECFCs across all groups.
Conclusion:
Despite clear differences observed in the gross images of plugs, no significant differences were seen following microscopic quantitation. This was possibly due to the small sample size per group and the marked variability between data points. However, considering the data reported above, the findings appear to highlight a potential inhibitory role of VWF in angiogenesis. Further experimentation is required to establish whether localized VWF can reverse the proangiogenic phenotype observed in VWF-deficient mice.
Disclosures
James:Band Therapeutics: Consultancy; Bayer: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.