Abstract
Title: T-Lymphocyte Subset (CD25+) And Response To Therapy In Immune Thrombocytopenia
K Mishra,1 S Kumar,1 KJ Singh, P Tripathi,2 S Rashid,3 B Revanth,1 R Kapoor,1
Introduction: Immune thrombocytopenia (ITP) is the commonest autoimmune bleeding disorder. Autoantibody-mediated destruction of platelets with or without bone marrow suppression of megakaryocytes is the most widely implicated etiology. Corticosteroid is the first-line therapy. However, not all patients respond to the corticosteroid and many of the responders relapse soon after the stoppage of corticosteroids. CD25 positive T-lymphocyte subsets (T-reg) are known to modulate the immune response, thereby ensuring homeostasis and maintaining self-tolerance. Flow cytometry is easily available, reasonable quick, and economical investigation around the world. We aimed to estimate the Treg population by flowcytometry in patients of ITP and evaluate the response to therapy.
Methods: The study was conducted at the department of clinical hematology, medical division, Army Hospital (Research and Referral), New Delhi, India. In this prospective observational study, patients with ITP (newly diagnosed or relapsing), requiring therapy, with or without active bleeding were included. All these patients were clinically evaluated and samples were collected as per unit protocol for ITP. For the Treg subpopulation, fresh blood samples were drawn in a heparinized vacutainer. CD4 and CD25 positive T-lymphocytes were estimated as Treg population by flowcytometry (NAVIOS EX Beckman coulter).
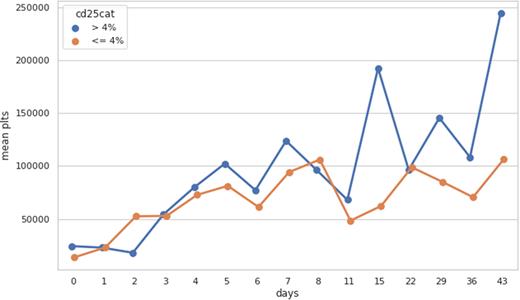
Results: A total of forty patients were included in this study. For analysis, patients were divided into two groups based on CD 25 cells population (Group-A > 4% Treg, and Group B < 4% Treg). There were 25 patients in Group-A and 15 patients in Group-B. Both the groups were matched in terms of patient age, diagnosis, and platelet count. All patients received corticosteroid therapy. After therapy, the mean platelets at day 30 in Group-A was 142428/cmm and in Group-B was 85000/cmm. The response (platelet rise) in Group-A was marginally better on day seven of therapy but it was statistically not significant. However, the response in Group-A was significantly better on day thirty of therapy (p=.042) (Figure 1).
Conclusion: The study signifies the importance of Treg cells in predicting the response to corticosteroids in adults. The patients who have Treg (CD25+) cells < 4% are expected to have a poor response to corticosteroid alone. Therefore, further study should be done to explore the possibilities of second line therapy or combination therapy in such patients.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.