Abstract
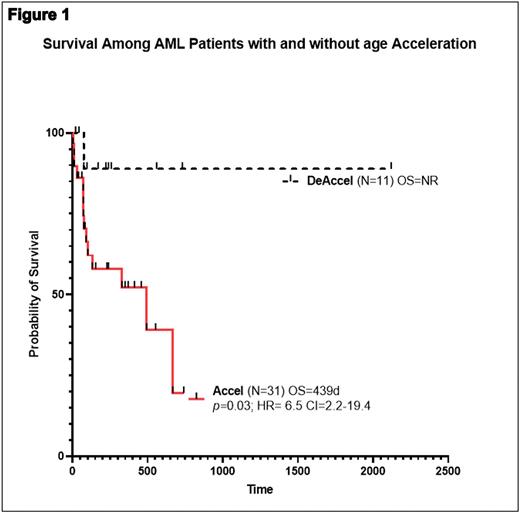
Background: Aging is strongly associated with hematologic malignancies. Chronological age (CA) fails to explain biological and clinical outcome differences among AML patients (pt) at same age. Phenotypic age (PA) has gained momentum to predict cause-specific mortality in individuals sharing similar CA. Age acceleration (AA), resulting from the difference between phenotypic or methylation age (MA) and CA correlates with all-cause mortality. Similarly, Clonal Hematopoiesis of indeterminate Prognosis (CHIP) is associated with AA [PMID: 34050697]. CHIP mutations (mut) may be inherited into AML from preexisting immortalized/transformed cells. Cells harboring CHIP induce inflammation and "accelerate" vascular complications [i.e coronary artery disease (CAD)]. In this study, we seek "proof of clinical concept" for an association between AA and AML outcome when accounting for the presence or not of CAD. Methods: After IRB approval, AML pt were selected to estimate PA based on "proposed score 9 clinical biomarker's score" [PMID: 29676998] including albumin, creatinine, glucose, c-reactive protein, lymphocyte percent, red cell mean cell volume, red distribution width, alkaline phosphatase, white blood count). PA was calculated at AML onset. Difference between PA and CA was recorded as Delta PA-CA. Positive and negative delta PA-CA were considered as AA vs rejuvenation. Given the association between inflammation, CAD and CHIP, we performed individual correlation survival analysis accounting for phenotypic age in AML pt with and without CAD. Descriptive statistics, univariate and multivariate analysis were performed using SAS software. Results: 81/253 (32%) AML pt were available. Pearson correlation revealed that in pt without CAD, PA negatively correlated with survival (R= -0.31, p= 0.04), an effect not observed among AML pt with established CAD (R= -0.10, p=0.52). With AML pt lacking CAD [42/81(51%)] representing our population of interest, median CA, PA and MA among pt with (N=31) or without (N=11) AA was 53 years (y) v 49, p=0.5, 84 v 44, p= 0.0001 and 79 v 44, p=0.0001. WBC was 27 K/uL v 32.4 K/uL, p=0.5, in pt with and without AA. Favorable (fav) ENL-2017 was 33% vs 18%, p=0.1, Int 11% vs 18%, p=NS and unfav 56% v 64%, p=NS in pt with and without AA. Overall survival (OS) was 439 d vs not reached (NR), in pt with and without AA, p=0.03, HR=6.5 CI 2.2-19.4. Multivariate cox regression considering ELN-2017 classification, age and PA revealed that only AA was independent predictor of outcome, p=0.03, HR-1.02, CI=1.002-1.03. Conclusions: AA is associated with inferior AML outcome without overt CAD. In our proof of concept cohort, and acknowledging small sample size, AA supersedes ENL-2017 classification and CA as predictors of inferior outcome in AML. Our study adds insight on how AA based on epigenetic clock estimation potentially influences not only leukemogesis, but also renders organ function inability to survive AML.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.