Abstract
Background: Sickle cell trait (SCT) is found in nearly 3 million individuals in the United States, constituting 7% to 9% of the African American population. Worldwide, the number of individuals with SCT exceeds 300 million. SCT is generally an asymptomatic genetic carrier state, and most carriers never develop associated clinical complications. However, studies have reported clinical manifestations associated with carrier status in rare circumstances. The hematology community has called for increased epidemiological research on SCT, including large population-based studies.
Methods: This cross-sectional study uses data from the All of Us Research Program (AoU), an NIH program that seeks to build the largest and most diverse research database. This analysis utilizes electronic health records (EHR) and self-reported data to identify the difference in frequency of reported SCT-related clinical outcomes between a cohort of known SCT-carriers and a randomized matched sample of individuals without a known history of SCT.
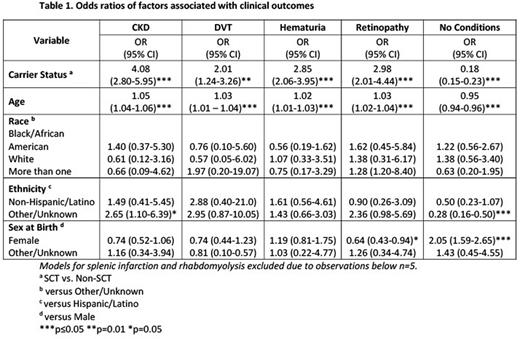
A total of 201,920 EHRs were reviewed and a cohort of 982 participants reported as SCT carriers were identified. A comparison group of individuals without a known history of SCT (n=982) matched on age range, sex at birth, and self-reported race was randomly selected from the AoU database. Individuals with sickle cell disease were excluded during the random selection of the comparison group. The prevalence of six conditions with varying strengths of evidence in association with SCT was assessed for both cohorts. Conditions were chosen in accordance with findings reported in a 2018 systematic review, Clinical Outcomes Associated with Sickle Cell Trait(PMID: 30383109). Selected conditions included chronic kidney disease (CKD), rhabdomyolysis, deep vein thrombosis (DVT), hematuria, retinopathy, and splenic infarction. Identification of condition diagnosis was based on reported Systemized Nomenclature of Medicine (SNOMED) codes within EHRs for both cohorts. Only the first occurrence of a reported condition for each participant was included in our analysis and duplicate reports were removed to properly assess frequency of each condition. Multivariate logistic regression was used to examine the association of each condition based on SCT carrier status.
Results: Participants within the SCT cohort (n=982) were predominantly Black/African American (68.3%), non-Hispanic (70.3%), female (83.2%), and had a mean age of 55 years (range 21-87 years). There was a significant association between reported diagnosis of all conditions and SCT carrier status (CKD (OR= 4.08, 95% CI= 2.80-5.95), DVT (OR= 2.01, 95% CI= 1.24-3.26), hematuria (OR= 2.85, 95% CI= 2.06-3.95), and retinopathy (OR= 2.98, 95% CI= 2.01-4.44)). Models for splenic infarction and rhabdomyolysis were not fit due to insufficient observation counts. Age was also found to be significantly associated with reported diagnosis of all conditions, each with a p-value ≤ 0.05. Regardless of carrier status, female participants had lower risk of a reported diagnosis of retinopathy (OR= 0.64, 95% CI= 0.43-0.94) compared to men. No significant association between race and ethnicity and reported diagnosis of conditions was found.
Conclusion: In this case-control analysis using recorded SCT status, SCT was associated with CKD, DVT, hematuria, and retinopathy. This is the first large study to suggest an association between SCT and retinopathy. Further analysis of this cohort using direct genotypic data for SCT will be critical to better characterize these associations.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.