Abstract
Background: Red-cell exchange (RCE) is a mainstay of treatment for both acute and chronic complications of sickle cell disease (SCD). It is a resource-intensive intervention requiring transfusion of large volumes of antigen-matched red blood cells (RBC). Identifying suitable RBC units can be challenging due to variability in blood group phenotypes between patients with SCD and the donor population. This often results in use of O-negative units, which are a scarce resource. Efforts to reduce the volume of units transfused, while maintaining therapeutic efficacy is an important clinical need. Isovolemic hemodilution (IHD) prior to RCE reduces the required volume of RBCs. The aim of this project is to evaluate the effect of a change to IHD-RCE on RBC utilization in patients with SCD receiving standard RCE.
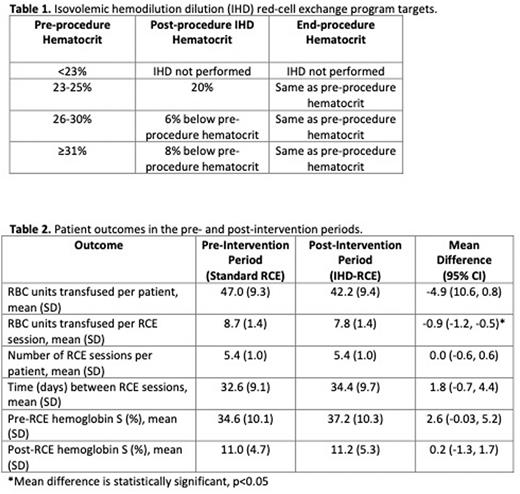
Methods: All adult SCD patients receiving standard RCE at the Ottawa Hospital were identified. To safely attain a meaningful reduction in transfused RBCs, RCE treatment parameters were individualized for each patient (Table 1). Patient hematocrit was not allowed to decrease below 20% during the depletion phase, and IHD-RCE would be performed only if an estimated reduction in RBC volume of at least 200 mL was expected. Pregnant patients were excluded. Change in RCE protocol to IHD-RCE took place in January 2022. Transfusion and clinical data were obtained from databases at the Ottawa Hospital in the six months preceding and succeeding the change in RCE protocols to allow for a pre- and post-intervention comparison.
Results: Thirty-four adults receiving regular RCE for SCD were identified. Twenty-two patients met criteria for a protocol change to IHD-RCE. The mean age of the IHD-RCE cohort was 31 years (SD 9.5). Males comprised 72.7% of this cohort, with the most frequent genotype of hemoglobin SS (68.2%). Over the one-year study period, 1963 RBC units were transfused: 1035 RBC units in the pre-intervention period, and 928 units in the post-intervention period, representing a reduction of 107 RBC units. 1958 (99.7%) of the RBC units transfused were transfused in the setting of RCE, with few (5 units; 0.03%) administered as simple RBC transfusions. Table 2 outlines patient outcomes during the study period. The mean number of RBC units transfused per patient in the pre- and post-intervention periods were 47 and 42.4 units, respectively. The mean number of RBC units per RCE session per patient was significantly reduced from 8.7 units in the pre-intervention period to 7.8 units in the IHD-RCE post-intervention period (mean difference: -0.9, 95% CI: -1.2 to -0.5). A total of 236 RCE sessions occurred during the study period. No difference in RCE session frequency was observed with a change to IHD-RCE during the six-month study period, nor time between RCE sessions. Therapeutic efficacy in attaining target hemoglobin S levels was not affected by the change to IHD-RCE. No adverse patient safety signals were observed during the IHD-RCE sessions to date.
Conclusions: This study demonstrates that IHD-RCE, compared to standard RCE, substantially reduces RBC utilization. A total of 107 RBC units were conserved in our patient cohort of 22 chronic RCE patients directly from the transition to IHD-RCE from standard RCE. Based on local RBC per unit costs, this corresponds to an annualized saving of $95,444 CAD. With pressure on blood banks to provide appropriately matched units, and risks of alloimmunization and delayed hemolytic transfusion reactions amongst chronically transfused SCD patients, increased uptake of IHD-RCE should be considered for SCD patients on chronic RCE.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.