Abstract
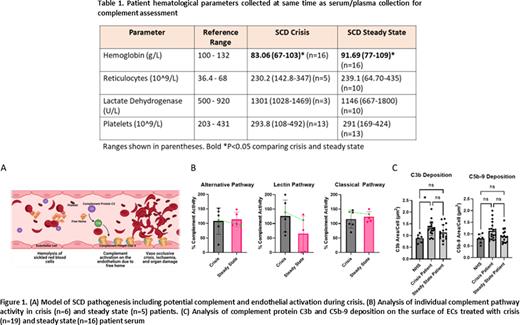
Background: Sickle cell disease (SCD) is one of the most common life-threatening hereditary red blood cell (RBC) disorders, with an estimated 300,000 infants born annually with the disease. In SCD, a mutation in the gene for β-globin results in rigid sickled RBCs that have difficulty navigating the vasculature and increased risk for forming blockages in the micro-vessels within organs, leading to RBC lysis, endothelial cell (EC) damage, ischemia/reperfusion injury, and extremely painful vaso-occlusive crises (VOC). Overtime, this can lead to stroke, serious organ damage, and other complications, resulting in a reduced life expectancy. Emerging research points to the involvement in SCD of complement, an important part of the innate immune system composed of proteins that are activated to help clear invaders and damaged cells from the body. Recent work by others has demonstrated that complement activation occurs in patients with SCD in both acute and chronic phases of the disease, and may be associated with disease severity and VOC (Fig 1A). This study aims to assess the role of complement activity in children with SCD during acute crisis and disease steady state.
Methods: Pediatric patients aged 0-18 with SCD (HbSS or HbS/β0) managed at The Hospital for Sick Children (Toronto, Canada) were enrolled in this REB approved study during hospital admission with diagnosed VOC or acute chest crisis (ACS) not caused by infection. Patient serum and plasma was collected during hospital admission (crisis) and during follow-up (steady state, 3 to 12 months following an acute crisis) simultaneously with routine bloodwork. Patients with >3 crisis admissions in the previous 12 months or requiring admission for >7 days were excluded. Pooled normal human serum (NHS) was collected from healthy volunteers for use as a control. Complement activity was measured using the WIESLAB Complement System Screen (Svar Life Science). Immunofluorescence (IF) imaging was used to measure the deposition of C3b and C5b-9 complement proteins on the surface of ECs exposed to patient serum or NHS. Data were analyzed using an unpaired t-test or one-way ANOVA with Tukey's multiple comparisons.
Results: Thus far, 58 patients have been enrolled in the study. SCD crisis patients showed significantly decreased hemoglobin compared to steady state (Table 1). Complement activity was assessed for 6 crisis and 5 steady state patients. There was equal classical and alternative pathway activity during disease steady state and crisis, which indicates no in vivo complement protein depletion in patients, with an interesting trend showing elevated MBL pathway activity during crisis compared to steady state (Figure 1B). Complement deposition was assessed via IF in 19 crisis, 16 steady state patients, and 6 replicates of NHS. IF assay data show significantly elevated deposition of C3b on ECs when comparing patient crisis samples and healthy controls, with trends suggesting a potential difference in C5b-9 deposition between NHS and crisis patients, as well as differences in complement deposition between steady state and crisis patients (Fig 1C).
Conclusion: Our preliminary data shows complement is active in SCD, resulting in elevated C3b deposition on ECs during SCD crisis. Although not statistically significant, trends suggesting a difference in C5b-9 deposition and differences between steady state and crisis patients are encouraging, as a small change in intravascular complement activity may still have significant physiological consequences. Future work is focused on further quantifying complement activity and understanding its mechanism, assessing the in vitro functional consequences of this on the surface of ECs, and investigating complement blockade as a potential treatment.
Disclosures
Kuo:Alexion: Consultancy, Honoraria; Celgene/BMS: Consultancy; Apellis: Consultancy; bluebird bio: Consultancy; Pfizer: Consultancy, Research Funding; Novartis: Consultancy, Honoraria; Bioverativ/Sanofi/Sangamo: Membership on an entity's Board of Directors or advisory committees; Agios: Consultancy, Membership on an entity's Board of Directors or advisory committees. Licht:Apellis: Honoraria; Catalyst Biosciences: Honoraria; Eleva: Honoraria; Novartis: Honoraria; Fresenius: Research Funding; Pfizer: Research Funding; Alexion, AstraZeneca Rare Disease: Honoraria, Other: Canadian coordinator for trials of eculizumab in patients with aHUS that were funded by Alexion, AstraZeneca Rare Disease; Global aHUS registry: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.