Abstract

BACKGROUND: Immune thrombotic thrombocytopenic purpura (iTTP) survivors are at increased risk cardiovascular events including stroke, which is associated with low remission ADAMTS13 activity. In the prospective Neurologic Sequelae of TTP (NeST) study, we evaluated the prevalence of silent cerebral infarction (SCI, ischemic lesions on brain MRI without overt neurodeficits that are a risk factor for future stroke), identified risk factors for SCI, and examined the association of SCI with cognitive impairment, which is prevalent in iTTP survivors.
METHODS: We prospectively enrolled adult (age ≥ 18 years) patients with iTTP based on ADAMTS13 activity <10% during an acute episode. All study assessments were performed after achieving hematological remission. Participants undergo annual study visits that include: 1) Brain MRI: SCI is defined as a infarct like lesion (punctate T2 and FLAIR hyperintensity) ≥3 mm in size without corresponding neurodeficits., 2) NIH ToolBox Cognition battery, an extensively-validated tool that tests multiple cognitive domains including executive function (dimensional change card sort test, flanker inhibitory control and attention test), processing speed (pattern comparison test), episodic memory (picture sequence memory test), working memory (list sorting working memory test), language (oral reading recognition, picture vocabulary test). Fully-corrected T scores (normative mean 50, SD 10) adjusted for age, sex, race and educational attainment are computed for individual tests as well as composite scores for fluid cognition, crystallized cognition and total cognition. Mild and major cognitive impairment are defined as a T scores that are 1-2 SD below mean and > 2 SD below mean for any domain, respectively; 3) the Beck depression inventory was also completed since depression is a potential confounder that is common in iTTP and may contribute to impaired cognition.
RESULTS: Between September 2020 and July 2022, 39 iTTP patients were enrolled; 32 patients completed MRI (2 excluded due to metal implant/shrapnel, 4 stopped for anxiety/claustrophobia). Median age was 48 years, 71% were female, and 23% had previous stroke (including during acute iTTP).
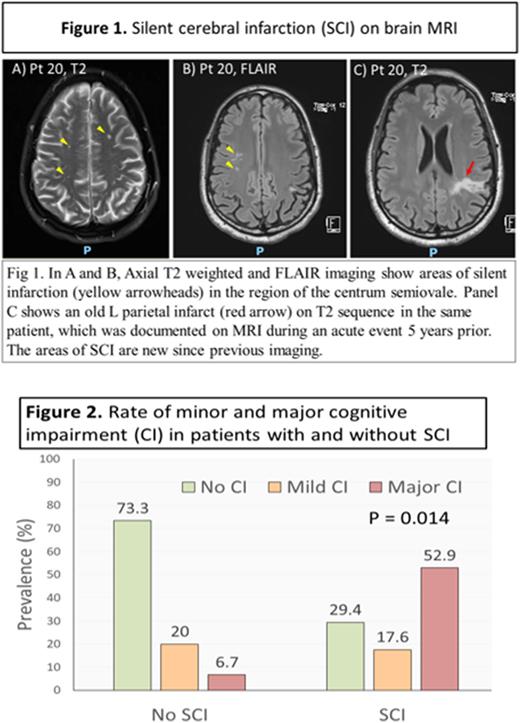
Prevalence and predictors of SCI: MRI showed SCI in 53.1% (Figure 1). Only 47% (8/17) patients with SCI had prior overt stroke. Age [OR 1.07 (95% CI 1.01-1.15, P=0.025) and history of stroke [OR 12.8 (95% CI 1.07-152.9), P=0.044] were associated with SCI in a logistic regression model adjusted for number of iTTP episodes [OR 1.14 (95% CI 0.71-1.86), P=0.570], hypertension [OR 0.77 (95% CI 0.14 - 4.25), P=0.768], and Black race [OR 2.10 (95% CI 0.16-28.20], P=0.574].
SCI is associated with cognitive impairment: Mild and major cognitive impairment were present in 23.1% and 30.8%, respectively. Deficits most commonly involved executive function (flanker inhibitory control and attention test, dimensional change card sort test) and processing speed (pattern comparison test). Compared to patients without SCI, those with SCI had higher rates of cognitive impairment (70.5% vs. 26.7%) including major impairment (52.9% vs. 6.7%) (P=0.014) (Figure 2). In logistic regression models adjusted for age and prior stroke, SCI was associated with major cognitive impairment [OR 18.13 (95% CI 1.3-259.1), P=0.033] as well as mild cognitive impairment [OR 7.76 (95% CI 1.03-58.29]. Patient with SCI had lower composite scores on the NIH ToolBox cognition battery [fluid cognition composite 41 vs. 55, P=0.009, crystallized composite 50 vs. 60, P=0.033, total composite 46 vs, 59, P=0.004), as well as lower scores on tests of executive function (flanker inhibitory control and attention, P=0.020) and processing speed (pattern comparison test, P=0.004), which are most commonly affected in iTTP.
Patients with SCI did not have higher mean Beck Depression inventory scores (12.0 ± 7.8 vs. 11.67 ± 11.5, P = 0.659) than those without SCI suggesting that the association with cognitive performance is not due to higher rates of depression in this group.
CONCLUSIONS: MRI evidence of brain infarction is common in patients with iTTP with or without a clinical history of stroke. Ongoing follow up with serial MRI continues and will inform whether SCI are progressive in remission and whether low remission ADAMTS13 is a targetable risk factor. The strong association of SCI with impaired cognition suggests that these 'silent infarcts' are neither silent nor innocuous.
Disclosures
Gerber:Pfizer (spouse): Current Employment, Current equity holder in publicly-traded company, Divested equity in a private or publicly-traded company in the past 24 months. Streiff:Pfizer: Honoraria; NovoNordisk: Research Funding; Tremeau: Research Funding; CSL Behring: Honoraria; Sanofi-Aventis: Research Funding; Janssen: Honoraria. Naik:Elsevier: Consultancy. Lanzkron:HRSA: Research Funding; PCORI: Research Funding; CSL-behring: Research Funding; Takeda: Research Funding; GBT: Research Funding; Novartis: Research Funding; Imara: Research Funding; Glycomimetics: Consultancy; Novartis: Consultancy, Research Funding; Pfizer: Consultancy, Current equity holder in private company; Novo Nordisk: Other: Adjudication committee; bluebird bio: Other: Adjudication committee, Research Funding; Teva: Current equity holder in private company. Braunstein:Incyte: Current Employment. Brodsky:Alexion: Honoraria. DeBaun:Novartis, GBT, Vertex, and Forma Pharmaceutical: Consultancy, Research Funding. Chaturvedi:Sanofi Genzyme: Honoraria; Takeda: Honoraria; UCB: Honoraria; Argenx: Honoraria.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract
Asterisk with author names denotes non-ASH members.