Abstract
Background
Patients with MGUS can progress to LPN. Non-IgG subtype and the size of the M-band are known to correlate with the risk of progression. Consensus guidelines recommend that patients be monitored on an annual basis, but that IgG MGUS with an M-band < 1.5 g/dL, and a normal serum free light chain ratio is at low risk and can be managed with less intensive monitoring. There are limited data on the risk of progression to LPN in non-IgG MGUS with small M-bands.
Methods
Kaiser Permanente Northern California (KPNC) is a large integrated health care system serving more than 4 million members representative of Northern California residents. We identified a cohort of 3,303 KPNC health plan members who had at least one serum protein electrophoresis (SPEP) performed between January 1997 and December 2006 and extracted follow up data through December 2016. We excluded those with an M-Band > 3 g/dL, absence of a confirmatory immunofixation, or LPN before through 3 months after initial SPEP. The primary end point was progression to LPN, defined as multiple myeloma (MM), non-Hodgkin's lymphoma, or amyloidosis, and identified via an integrated tumor registry and, in the case of amyloidosis, by clinic diagnosis.
Findings
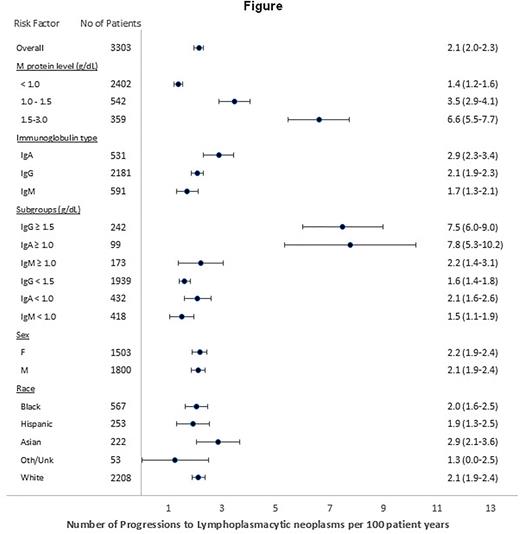
The median age of this cohort was 73 (IQR 63-80), 54.5% were male, and the ethnicity of this group was White 66.9%, Black 17.2%, Asian 6.7%, Hispanic 7.7%, and others 1.6%. Sixty six percent had an IgG gammopathy and 73% of gammopathies were < 1.0 g/dL. Overall, there were 2.1 (2.0-2.3) progressions per 100 patient years. The number of progressions per 100 patient years for an M-band < 1.0 g/dL, 1.0-1.5 g/dL, and 1.5-3.0 g/dL were 1.4 (1.2-1.6), 3.5(2.9-4.1), and 6.6 (5.5-7.7) respectively. As can be seen in the Figure, the cumulative risk of progression to LPN was clinically similar for patients with an IgG ≥ 1.5 g/dL and IgA ≥ 1.0 g/dL and considerably increased compared to those with an IgG gammopathy < 1.5 gm/dL, IgA gammopathy < 1.0 g/dL, or an IgM of any size.
Discussion
It has been estimated that there are several million individuals in the United States with MGUS. Following a patient with MGUS indefinitely is a financial burden and creates a substantial psychologic burden for the patient. Others have found that the effect of an MGUS diagnosis on quality of life is greater than a new diagnosis of symptomatic MM. Therefore, identifying additional categories of MGUS that could be assigned to a low-risk category could potentially diminish the burden and stress of ongoing monitoring.
Limitations of our study are that, owing to the period from which our cohort was accrued, and the nature by which they were identified, free light chain levels were not obtained, bone marrow biopsies were done infrequently, and modern advanced imaging was not performed. In the modern era, many of our cohort would likely be identified with more advanced neoplasia such as smoldering or frank MM accounting for the higher rates of progression compared with other published reports.
We found that during much of the period covered by our study, the clinical diagnosis of Waldenstrom's Macroglobulinemia was used in a non-discriminatory manner. We therefore limited our definition of progression only to those subjects developing frank malignancy that qualified for inclusion in our tumor registry rather than the less rigorously defined entity of "Waldenstrom's Macroglobulinemia.". This likely accounts for the lower risk of progression to LPN among our cohort with IgM gammopathy than has been described elsewhere.
Conclusion
Patients with either IgM MGUS of any size or IgA MGUS with an M-band < 1.0 g/dL have an equivalent clinical risk of progression as patients with an IgG MGUS < 1.0 g/dL and should potentially be assigned to a low-risk category to decrease the burden and stress of ongoing monitoring.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.