Abstract
Background: Bloodstream infection (BSI) is a lethal complication in hematologic patients with febrile neutropenia (FN). The delayed diagnosis and intervention will lead to significant mortality. Unfortunately, the traditional golden standard diagnostic method using blood culture (BC) can only identify pathogens in 20-30% patients with BSI, and usually needs more than 48 hours. Therefore, novel methods with fast turnover, improved sensitivity and specificity are needed. Metagenomics next-generation sequencing (mNGS) shows promise as diagnostic testing for difficult and critical infectious diseases in immunodeficient hosts, but its significance in BSI of hematological patients remains unclear, and has not been evaluated in prospective study.
Aims: To evaluate the ability of mNGS to identify infectious etiologies in FN patients with BSI.
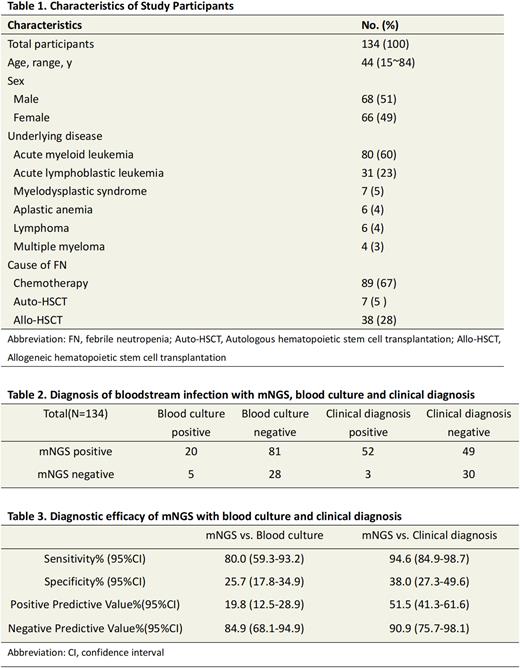
Method: This study was prospective performed in four Chinese hematologic centers since October 2021. For patients≥15 years with hematologic diseases, patients were screened at the onset of neutropenia. At the onset of FN, Peripheral blood specimens were collected per subject for simultaneous BC and mNGS (separate sequencing for plasma and blood cells). All patients will be followed for 14 days, or until death before 14 days. The intervention was per the attending physician. The primary endpoints of this study is the sensitivity and specificity of mNGS. Thepositive agreement was defined as mNGS identified at least one same pathogen as initial BC. The negative agreement was defined as both mNGS and BC were negative. And the adjudication of the result of BC, mNGS, and clinical diagnosis was evaluated by 4 independent specialists in hematology. Clinical adjudication categorized mNGS results as: Definite, mNGS identified at least one pathogen also found by BC or SMT with in 7 days; Probable, mNGS result was concordant with a clinical diagnosis of BSI in FN; Possible, mNGS result was consistent with BSI but not considered a common cause of FN; Unlikely, mNGS result was not a plausible cause of BSI in FN. This study was registered on ClinicalTrials.gov ID: NCT05149547. This is an interim analysis of 134 patients enrolled in this multicenter, prospective observational study.
Results: Te basic information of the patients was summarized in table 1. Clinical adjudication categorized mNGS results as: Definite (N=24); Probable (N=21); Possible (N=7); Unlikely (N=49). Definite, probable and possible cases were regarded as true positives. The positive percent agreement (PPA) and negative percent agreement (NPA) with BC were 80.0% (20/25) and 25.7% (28/109) respectively; 44% of mNGS results were polymicrobial (except viruses). According to the clinical adjudication, mNGS sensitivity and specificity were 94.6% (52/55) and 38.0% (30/79) respectively (table 2 and table 3). Compared with BC, the reporting time of mNGS was significant shorter (24.8±4.0 vs. 72.3±21.2 h, p < 0.05).
Conclusions: Compared with conventional BC, mNGS might provide an early and rapid microbiological diagnosis of BSI in hematologic patients with FN. However, the clinical application needs pending further study.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.