Abstract
Title: Evaluating anemia related morbidity in premenopausal female minority and disadvantaged populations
Authors: Alexander Krule, M.D. M.S., Kristy Abraham, M.D., David Dulce, Sandra Cuellar Puri Pharm. D., Ameen Salahudeen, M.D. Ph.D., Amina Chaudhry, M.D.
Introduction: In the United States, there are pronounced racial disparities in anemia prevalence among adult women under 50 years of age with 3.3% of white, 8.7% of Latina, and 24.4 % of Black women affected. The most common etiology of this anemia is iron deficiency anemia (IDA) affecting up to 12% of reproductive-aged American women across all racial groups with a disparate increased burden of IDA among Black women where 19% have iron deficiency. This presents an opportunity for multimodal interventions for patients and the medical community to improve health outcomes in women with iron deficiency anemia. The purpose of this study is to assess the severity and burden of iron deficiency anemia in the Black versus non-Black communities at University of Illinois (UI Health).
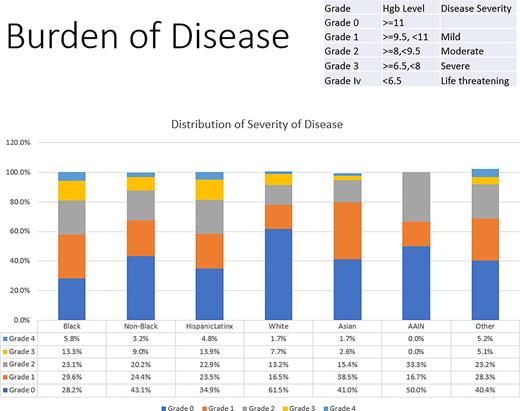
Methods: We underwent a retrospective chart review of patients at UI Health with anemia from 1 June 2011 - 21 May 2021. Included patients were 18-40 years old, listed female sex in their charts, and had a diagnosis of iron deficiency anemia defined as serum hemoglobin less than 12 mg/dL and serum ferritin less than 30 ng/mL or transferrin saturation less than 19%. Exclusion criteria were male sex, amenorrhea, induced menopause, primary ovarian insufficiency, history of bariatric procedures circumventing the duodenum, autoimmune disease, and heart failure. In total, 951 patients with iron deficiency anemia were identified, of which 756 met criteria for analysis. We then grouped patients by listed race and ethnicity and stratified patients by severity of anemia as defined by the World Health Organization (WHO). WHO anemia severity grades anemia based on hemoglobin ranging from Grade 0 for hemoglobin values within reference range to Grade III and Grade IV for severe and life-threatening hemoglobin values below 7.9 and 6.5 g/dL, respectively. Statistical differences between groups were analyzed by ANOVA and logistic regression models.
Results: Of the 756 patients included in the analysis, 68% identified as Black, 21% as Latinx, 12% as White, 5% as Asian, and 0.7% as American Indian/Alaskan Native. A one-way ANOVA revealed that there was a statistically significant difference in mean hemoglobin values between groups. Testing of the a priori hypotheses were conducted using Bonferroni adjusted alpha levels of .0125 (0.5/4) per test and showed a significantly lower mean serum hemoglobin for Black patients (M=9.7, SD=0.6) than non-Black patients (M=10.4, SD=0.4, F(4,1242)=14.8, p<10-11). In an unadjusted logistic regression model, Black race was significantly associated with more severe degree of anemia compared to non-Black race (OR=1.79, 95% CI [1.38,2.32]).
Conclusion: More than two-thirds of female patients of reproductive age in the UI Health patient population with iron deficiency anemia self-report as Black. Black patients in this population have clinically significant lower hemoglobin levels than non-Black patients, and have a significantly increased hazard ratio for severe anemia. In our health system, symptomatic patients with severe and life-threatening anemia require emergent blood transfusion as standard of care, incurring further risk of morbidity and potentially mortality. Given the disparity we observe, and increased hazard for severe and potentially life-threatening anemia warrants further assessment into the delivery of healthcare to this underrepresented patient population. Evaluating what barriers may exist in delivering care to IDA patients in screening, diagnosis, and management of oral versus parenteral iron therapy should also be further studied.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.