Abstract
Physical activity has been shown to be beneficial for healthy individuals as well as cancer patients. In fact, scientific evidence suggests that it can reduce cancer related mortality. Yet, since bone destruction is a frequent symptom of multiple myeloma (MM) patients, they and their treating providers might try to limit physical activity to prevent further damage. Assessing how patients with monoclonal plasma cell disorders feel about physical activity, how much their participation has changed since diagnosis and how it influences their quality of life could provide evidence to develop future prospective studies. To investigate these questions, the online platform HealthTree® Cure Hub (HealthTree Foundation, Lehi, UT) was used to ask patients with monoclonal plasma cell disorders to report on recent (5 year before diagnosis), current and desired future physical activity. Increments of 0, 0-2, 2-4, 4-6 and >6 hours per week were used. Furthermore, patients were asked to fill in the following questionnaires: Visual Analogue Scale for Pain, EORTC QLQ-FA12 Fatigue Questionnaire, NCCN Distress Thermometer. Differences in means were analyzed using one-way ANOVA, between-subjects design for the overall effect, with Tukey's HSD test of differences between each diagnosis group. Differences in proportion of categorical variables were tested using chi-squared test of independence. Total categorical values may not sum to 100% due to missing data and rounding.
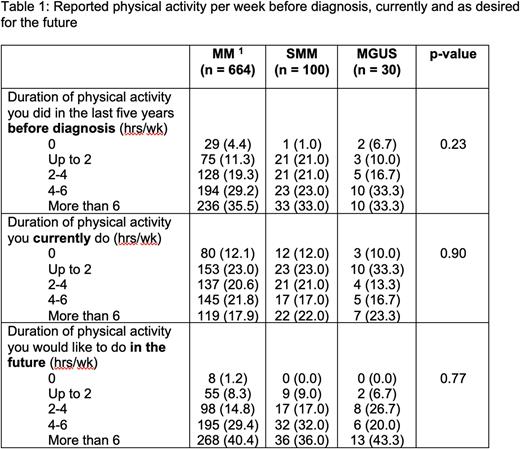
Between December 2019 and April 2022, a total of 794 individuals responded to the physical activity questionnaires. Of this cohort 664 patients reported to have been diagnosed with MM, 100 had SMM and 30 had MGUS. The mean age was 65.2 years for MM, 64.3 years for SMM and 64.0 years for MGUS patients. The mean age at diagnosis was 60.0, 60.6 and 59.3 years respectively, representing a rather younger cohort for this disease group. In total 54.4% (MM) 60.0% (SMM) and 73.3% (MGUS) of participants were female. The majority of patients were Caucasians (MM 83.1%, SMM 81.0%, MGUS 80%) and 3.0%, 5.0% and 6.7% were African Americans. Table 1 shows the reported hours of physical activity per week. Overall, patient reported that they had a reduction in active hours since diagnosis and that they would like to increase their time of being physically active. Not surprisingly active subjects also had a lower BMI (25.4 kg/m2) than low active (27.0 kg/m2) or inactive (30.2 kg/m2) subjects (p<0.01) and were more likely than low active or inactive subjects to be male (51.1% versus 40.0% and 36.2%, respectively, p<0.01). Education level was also higher in high active participants with 43.8% having a graduate or professional degree, versus 33.9% and 17.9%, respectively (p<0.01)
Active subjects were also more likely to get 7-8 hours of sleep per night (55.6% versus 47.1% and 34.7%, respectively, p<0.01) and to have not experienced a change in their sleep since before their diagnosis (60.3% versus 55.5% and 41.1%, respectively, p=0.02). Active subjects of any diagnosis were significantly more likely to respond "not at all” to all 12 fatigue questions than low active or inactive subjects, with a generally inverse relationship between these measures of fatigue and activity level (all p<0.01). Active subjects of any diagnosis had lower overall distress scores than low active or inactive subjects (51.4% versus 31.3% and 29.5%, respectively, reporting a score of 1-2, p<0.01).
In conclusion, patients with monoclonal gammopathies experience a reduction of their physical activity. The time per week of being physically active correlates with markers of quality of life. Ongoing prospective studies will address the cause and result relationship of these findings.
Disclosures
Hillengass:Skyline: Membership on an entity's Board of Directors or advisory committees; BMS: Membership on an entity's Board of Directors or advisory committees; Sanofi: Membership on an entity's Board of Directors or advisory committees; Oncotracker: Membership on an entity's Board of Directors or advisory committees; Oncopeptides: Membership on an entity's Board of Directors or advisory committees; GSK: Membership on an entity's Board of Directors or advisory committees; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: DSMB; Curio Science: Honoraria; Amgen: Honoraria; Beijing Medical Award Foundation: Honoraria; Beijing Life Oasis Public Service Center: Honoraria; Beigene: Honoraria; Axxess Network: Membership on an entity's Board of Directors or advisory committees; Adaptive: Honoraria. Ahlstrom:Pfizer, BMS, Janssen, Takeda Oncology, Sanofi: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.