Abstract
Background Allogeneic stem cell transplant (allo-SCT) for treatment of multiple myeloma (MM) is controversial. For some, allo-SCT may drive treatment-resistant disease into remission through a graft vs myeloma effect. For others, it incurs considerable morbidity from opportunistic infections and graft vs host effects. Allo-SCT usage for MM has increased over the past 25 years despite mixed efficacy and the absence of clear treatment guidelines. We aimed to determine the natural history of patients who underwent an allo-SCT following an autologous stem cell transplant (ASCT) and identify characteristics associated with outcome.
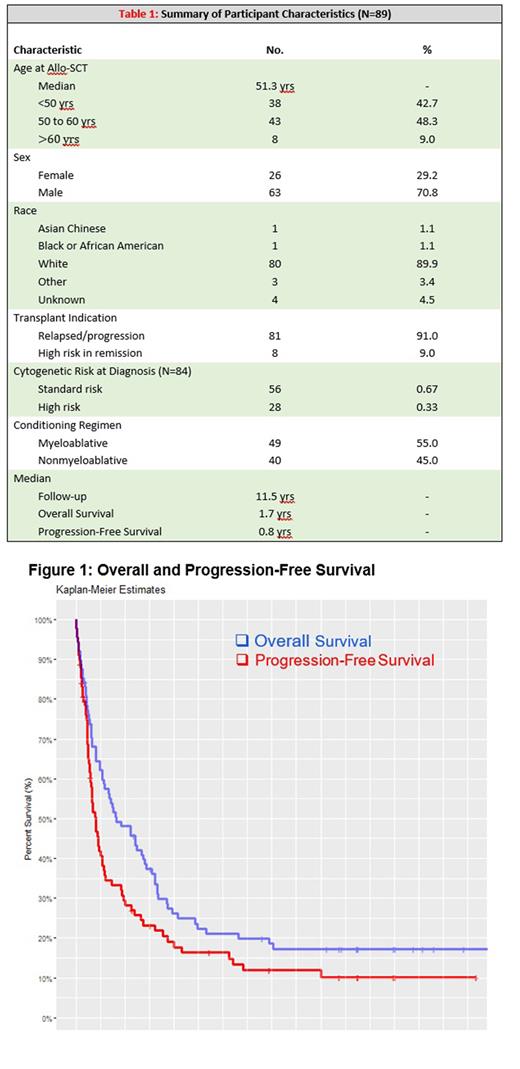
Methods We retrospectively analyzed 89 patients diagnosed with multiple myeloma who had received an allo-SCT following an ASCT between 2000 and 2022 at Mayo Clinic Rochester. Patient data were obtained from the Mayo Clinic Transplant Center Database and our institution's electronic medical records. Overall survival (OS) and progression free survival (PFS) were calculated as time from allo-SCT to death from any cause and first observation of relapse or death, respectively. OS and PFS rates were estimated using the Kaplan-Meier method. P < 0.05 was considered statistically significant.
Results The cohort is characterized as follows: median patient age of 51.3 years, 71% male, 90% white/Caucasian. Indication for allo-SCT were 91.0% (N=81) relapsed/progressive disease, 9.0% (N=8) high risk in remission. Cytogenetic risk stratification at diagnosis was available for 94% of patients (N=84) with 63% (N=56) standard risk, 32% (N=28) high risk according to International Myeloma Working Group criteria. By conditioning regimen, 55% (N=49) underwent full myeloablative allo, 45% (N=40) non-myeloablative (mini)-allo. Median follow-up, OS, and PFS was 11.5, 1.7, and 0.8 years, respectively (Table 1).
OS was 46% (N=41) at 2 years, 26% (N=21) at 4 years, and 16% (N=14) at 8 years (Figure 1). Outcome was not significantly impacted by age, sex, race, indication for allo-SCT, or myeloablative regimen. Patient cytogenetic risk at diagnosis approached, but did not reach, statistical significance (p=0.22) with overall survival of high-risk patients being 32% (N=9), 18% (N=5), and 7.1% (N=2) at 2, 4, and 8 years, respectively, compared to 52% (N=29), 27% (N=15), and 20% (N=11) over the same times in standard risk.
PFS was 27% (N=24) at 2 years follow-up, 16% (N=14) at 4 years, and 7.9% (N=7) at 8 years (Figure 1). This did not vary significantly by age, race, indication for allo-SCT, cytogenetic risk, or conditioning regimen. Sex approached, but did not reach, statistical significance (p=0.16) with progression-free survival of females being 19% (N=5), 15% (N=4), and 7.7% (N=1) at 2, 4, and 8 years follow-up, respectively, compared to males at 30% (N=19), 16% (N=10), and 9.5% (N=6) over the same times.
Discussion Long-term survival was achieved in less than 20% of patients who underwent allo-SCT following an ASCT. Nearly 75% of patients experienced disease progression or death by 2 years. This suggests minimal benefit to the use of allo-SCT as treatment for multiple myeloma outside of select patients. Novel therapeutics such as chimeric antigen receptor T cells (CAR-T) or bispecific T-cell engager (BiTE) should be considered as an alternative. Subsequent studies will further examine patient characteristics and associated outcomes to determine the population best suited for allo-SCT.
Disclosures
Kumar:AbbVie,: Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding; Janssen,: Membership on an entity's Board of Directors or advisory committees, Research Funding; Takeda,: Membership on an entity's Board of Directors or advisory committees, Research Funding; Adaptive,: Membership on an entity's Board of Directors or advisory committees, Research Funding; KITE,: Research Funding; MedImmune/Astra Zeneca,: Membership on an entity's Board of Directors or advisory committees, Research Funding; Merck,: Research Funding; Novartis,: Research Funding; Roche: Research Funding; Sanofi: Research Funding; Oncopeptides: Other: Independent review committee. Dispenzieri:Janssen: Membership on an entity's Board of Directors or advisory committees; Oncopeptides, and Sorrento: Other: Data monitoring safety committee; Alynlam, Pfizer, Takeda, and BMS: Research Funding. Dingli:Bristol Meyers Squibb Global Pharmaceutical Company: Consultancy; Alexion Pharmaceuticals: Consultancy; Apellis Pharmaceuticals: Consultancy; Novartis Pharmaceuticals: Consultancy; Roche: Consultancy; Sanofi: Consultancy; Regeneron Pharmaceuticals: Research Funding. Lacy:Celgene: Research Funding. Kapoor:Sanofi: Honoraria, Research Funding; X4 Pharmaceuticals: Honoraria; Regeneron: Research Funding; Amgen: Research Funding; Ichnos: Research Funding; Loxo: Research Funding; Karyopharma: Research Funding; BMS: Honoraria, Research Funding; AbbVie: Honoraria, Research Funding; Takeda: Research Funding; Casma: Honoraria; Pharmacyclics: Honoraria; Imedex: Honoraria; GSK: Honoraria; Cellectar: Honoraria; Oncopeptides: Honoraria. Leung:Takeda Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees. Muchtar:Protego: Consultancy; Janssen: Honoraria. Kourelis:Novartis: Research Funding. Gertz:Johnson & Johnson: Other: fees; Juno: Other: Meeting personal fees; Abbvie: Other: Personal fees for Data Safety Monitoring board; Sorrento: Other: Meetings personal fees; Celgene: Other: Fees; Ashfield: Other: Healthgrants and personal fees; Sanofi: Other: Personal Fees; Aptitude: Other: Personal fees; Janssen: Other: Personal Fees; i3Health: Other: Development of educational materials; Physicians Education Resource: Other: Personal fees; Prothena: Other: Personal Fees; Ionis/Akcea: Other: Personal Fees; Research to Practice: Other: Personal fees.
Author notes
∗Asterisk with author names denotes non-ASH members.