Abstract
Introduction: Sickle cell disease (SCD) results from a single mutation in the β-globin gene that causes hemoglobin polymerization, red cell sickling, vascular injury, and recurrent vaso-occlusive crises (VOC). Vascular protein disulfide isomerase (PDI) is shown to be critical for thrombus formation by facilitating neutrophil recruitment, platelet activation and vascular fibrin deposition, all processes implicated in sickle vasculopathy. Since plasma PDI is elevated in SCD and cell-surface associated PDI could promote tissue factor (TF) dependent thrombin generation, we investigated the effects of Isoquercetin (IQ) in patients with steady state SCD.
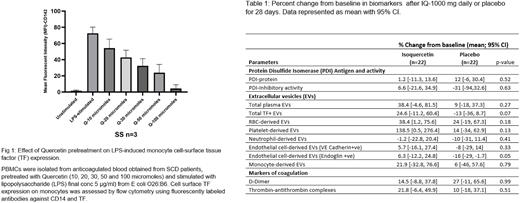
Methods: RBC surface associated PDI was quantified by western blotting. Inhibitory effect of IQ on LPS-induced TF expression on sickle monocytes in vitro was determined using flow cytometry. We also measured in vivo the effect of exposure of IQ or placebo for at least 28 days on plasma PDI protein, PDI reductase activity, total plasma extracellular vesicles (EVs), total plasma TF+ EVs, EV-TF-dependent procoagulant activity and markers of coagulation (D-dimer and Thrombin-antithrombin Complexes) using previously published methods. We used plasma from steady state SCD patients participating in a randomized controlled trial (NCT04514510) obtained at baseline and 28 days after exposure to either Isoquercetin 1000mg once daily (n=22) or placebo (n=22). The patients were in steady state, at least 60 days remote from VOC or blood transfusion and on a stable dose of hydroxyurea. The Wilcoxon rank-sum test was used to perform significance testing for differences in the percent change in outcomes between the Isoquercetin and placebo groups.
Results: Sickle RBCs had higher cell-surface associated PDI compared to ethnic matched healthy controls (fold change 5.09; p=0.028). In confirmatory experiments with RBC ghosts, extracellular PDI was cell-surface associated. Pretreatment with Quercetin (the active metabolite of Isoquercetin) reduced LPS-induced cell-surface TF expression on sickle monocytes in vitro in a dose dependent manner (Fig 1). Following Isoquercetin administration, there was no change in the percent reduction in PDI inhibitory activity in the IQ group (mean: 6.6, 95%CI [-21.6, 34.9]) compared to placebo group (mean; -31, 95%CI [-94, 32.6], p=0.63). The percent change from baseline in PDI antigen also did not differ between the IQ or placebo groups (IQ mean: 1.2, 95%CI [-11.3, 13.6]; placebo mean: 12, 95%CI [-6, 30.4], p=0.52) (Fig 1). There was no correlation between the percent change in PDI activity and antigen from baseline after treatment with IQ (Spearman's Rho, IQ: r2 =0.28; p=0.20 placebo: r2=0.10; p=0.67). Unexpectedly, total plasma EVs showed no difference between the IQ (mean: 38.4; 95%CI [-4.6, 81.5]) and the placebo group (mean: 9, 95%CI [-18, 37.3]; p=0.27) (Table 1) suggesting that IQ has no obvious anti-inflammatory effects. Moreover, plasma EVs were predominantly derived from RBCs and platelets as published previously by us and others, indicating no membrane stabilizing effect on sickle RBCs and platelets. Inhibiting PDI reductase activity could allosterically reduce TF procoagulant activity, but this hypothesis was untestable because the plasma EV-TF dependent procoagulant activity in this patient population was undetectable, possibly reflecting effective disease control by hydroxyurea.
Conclusions: The anti-inflammatory effects of flavonoid quercetin in vitro do not appear to translate into measurable clinical benefits in vivo following short term treatment with IQ in steady state SCD. Trials of higher dose IQ and/or prolonged exposure duration could yield greater inhibition of plasma PDI activity that might reveal detectable clinical antithrombotic effects.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.