Abstract
Background: The Central Hospital of the Instituto de Prevision Social (IPS) is the primary care point for 30% of the Paraguayan population. Patients with AML were treated on a general ward and had to change citizenship to receive allogeneic stem cell transplant (HSCT) abroad. Following the poor overall survival (OS) of the patients, a twinning program was started in 2015 with the help of the Worldwide network for Blood and Marrow Transplantation (WBMT). Physicians were trained at a JACIE/FACT accredited center for 6 months and the Hospital, staff, and nurses with an experience of 115 mostly autologous HSCT were inspected. The program started in 2016 by daily supervisory telemedicine visits including monitoring of vital signs, blood counts, chemistry and radiological analysis. In 2019, the need to improve treatment of AML prompted the Hospital to include newly diagnosed patients in the twining program. Now after 6 years, the outcome of AML patients was evaluated and compared to the results before the cooperation in 2012-2015.
Changes: One of the biggest challenges was the availability of essential drugs. Busulfan and several other preparative regimens and immunosuppressive drugs for HSCT were either not available or accessible only as oral formulation. Supportive therapy was a challenge considering lack of modern antifungal and antiviral therapy. To start the program, essential medications according to the WBMT recommendations were either donated from outside the country, included in the Insurance medications or ordered through the Ministry of Health. The allogeneic HSCT program was started using standard operating procedures (SOP) for central venous line care, neutropenia care, febrile neutropenia, transfusion threshold, visitors, patients per room, multidrug resistant bacteria active search and isolation of colonized patients, bacterial, viral, and fungal prophylaxis, and treatment. It was soon realized that only very few patients with AML survived induction therapy and reached CR. Therefore, the HSCT program started to include patients with AML from diagnosis in 2019. Newly diagnosed AML patients were therefore treated either on the conventional ward with 2-6 beds per room and common bathrooms or in the HSCT unit according to the availability of beds. SOP from HSCT patients were used for induction and consolidation treatments wherever possible. As quality control, OS was evaluated in the AML patients diagnosed in 2019-2021 according to treatment location and compared to the historical controls of 2012-2015 and to the HSCT patients.
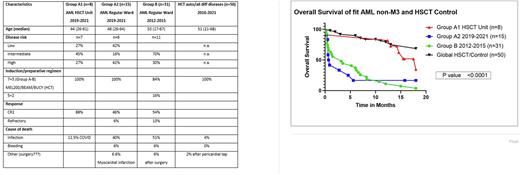
Results: Between 2019 and 2021, 23 patients received intensive chemotherapy induction, 8 patients in the HSCT Unit (Group A1) and 15 in the Regular Ward (Group A2). The controls included 31 historical patients with AML treated between 2012 - 2015 (Group B) and 50 patients after autologous or allogeneic HSCT between 2016-2021 (Group C). Patient`s characteristics are shown in Table 1. In comparison to the historical controls, diagnostics improved, and the treatment was given according to international protocols. Causes of death due to infection were reduced substantially to 12.5% in group A1 in comparison to 40% and 51% in group A2 and B, respectively. No bleeding fatalities were observed in Group A1 possibly because of strict transfusions according to SOP. In the HSCT control Group C only 4% died of infection and none of bleeding.
Figure 1 shows overall survival for all four groups. There were significant differences in median OS of the Group A1 (18 months), Group A2 (0,8 months), Group B (3,2 months) and Group C (not reached; p<0.0001). OS at 12 months amounted to 81% for Group A1, 15% for Group A2, 11% for Group B and 79% for Group C.
Conclusions: Improved survival following standardized treatment according to SOP can be achieved with strict adherence to protocols. Lower infection rate following isolation and standardized infection prevention and handling. Infection rate similar to the highest intensity of conditioning (autologous HSCT) and immunodeficiency (allogeneic HSCT). Even with the addition of new antifungal drugs and antivirals available at the regular ward between 2019-2021patients had low overall survival mostly due to bacterial infections following missing isolation, active surveillance, and prophylaxis. With this measures mortality following induction can be reduced effectively and is comparable to regular HSCT patients from developed countries.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.