Abstract
Background Prognostic risk stratification is crucial to individualize treatment in AML patients. The 2010 European Leukemia Net (ELN) classification grouped patients into 4 risk categories based on genetic alterations, which were redefinedinto 3 prognostic groups in 2017 taking into account new molecular data (TP53, RUNX1 and ASXL1).
Recently, ELN has proposed a new update considering additional prognostic mutations (such as SF3B1, SRSF2 and U2AF1)and removing ratio for FLT3-ITD. These ELN 2022 recommendations have not been validated yet in large cohorts of AML patients in real life.
Aims 1. Analyze the mutational landscape detected by Next Generation Sequencing (NGS) in consecutive real-life AML patients
2. Analyze whether the application of ELN 2022 risk model improves prognostic risk stratification compared to ELN 2010and 2017 and Medical Research Council (MRC).
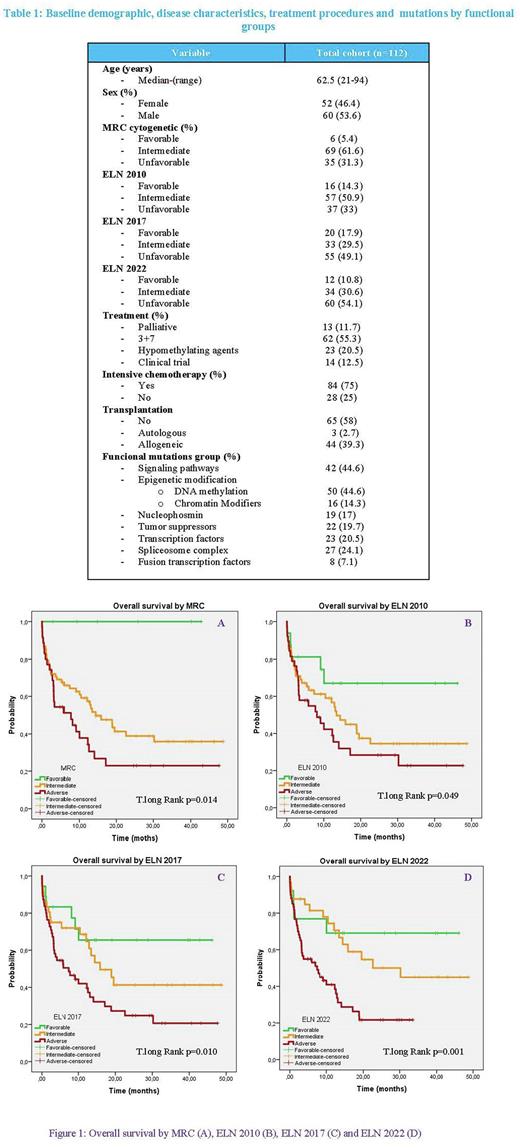
Methods We included 112 adult AML patients diagnosed in our center between June 2017 and December 2021 (Table 1) and who were studied at diagnostic using the Spanish PLATAFOLMA PETHEMA. The prognostic risk was established according to MRC, ELN 2010, ELN 2017 and ELN 2022 classification.
NPM1 and FLT3-ITD were determined by melting curve analysis and standard PCR-EC technique according to Thiede et al (Blood 2002) in ABI 3130 Analyzer (Thermofisher). For NGS, the commercial panel Myeloid SolutionTM (Sophia Genetics) KAPA Kit amplification libraries and sequencing on ILUMINA Myseq platform were used. Variant analysis was performed using DDM software (Sophia Genetics).
Results The majority of patients (97.1%) had at least one mutation at diagnosis detected by NGS. The median number of mutations was 2.4 (0-6). Grouped by functional genes, the most frequent were those related to DNA methylation (44.6 %) and signaling/kinase pathways (37.5%). The most prevalent were FLT3 (29 %), IDH1/IDH2 (27%) and TP53 (19.6%) followed by NPM1 and RUNX1 (17%).
Patients older than 60 years, presented higher percentage of unfavorable ASXL1 (18.6%), RUNX1 (20%) and TP53 (25.7%) mutations with respect to younger (4.8%, 11.9% and 9.5%) being these differences statistically significant in ASXL1 and TP53 (P=0.044 and P=0.047, respectively). NPM1 (28.6%) and FLT3 (40.5%) mutations were significantly more frequent in younger patients (P=0.017 and P=0.013, respectively), than in >60 years (10% and 17.1%, respectively).
Re-stratifying according to ELN2022, 32.4% of patients categorized within the intermediate risk group according to ELN 2017 change to adverse prognostic group and 13.2% in adverse risk group change to intermediate group due to the lack of impact of ratio for FLT3-ITD.
In the global series, the overall survival (OS) analysis shows statistically significant differences taking into account either ELN 2022, ELN 2017 or ELN 2010 and MRC (P=0.001,P=0.010, P=0.049 and P=0.012, respectively) (Figure 1). However, the greater differences between intermediate and unfavorable groups are found according to ELN 2022 compared to other classifications, and are also confirmed in patients receiving intensive treatment (P=0.021).Remarkably, patients receiving allotransplantation reverse adverse prognosis and enhance survival similar to intermediate group.
In our series, patients harboring mutations in signaling pathways genes (including FLT3) show better OS than those lacking, reaching statistical significance in allo-HSCT patients (P=0.037).
Summary/Conclusion 1. Our results validate the prognostic significance of the ELN2022 classification in real life, for the overall series and for candidates to intensive treatment.
2.ELN 2022 establishes greater survival differences between the unfavorable and intermediate group than ELN 2017or prior classifications. However, patients in adverse group undergoing allo-HSCT improve OS similar to intermediate group
3. FLT3 mutated allo-HSCT patients showed a strikingly low risk of relapse, partly due to the treatment with FLT3 inhibitors.
4. New studies including larger number of patients are needed to confirm our results.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.