Abstract
Background: Angioimmunoblastic T-cell lymphoma (AITL) is an aggressive subtype of peripheral T-cell lymphoma with a follicular helper T-cell immunophenotype. Up to 50% of AITL patients present with dermatologic manifestations. However, the prognostic implications of clinical, histologic, and immunophenotypic features of cutaneous AITL have not been fully elucidated.
Objective: To characterize clinical, histologic, and immunophenotypic features of cutaneous AITL and determine their prognostic significance.
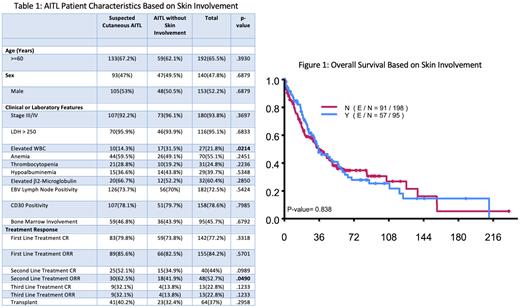
Methods: We identified 293 patients seen at our institution diagnosed with AITL by characteristic immunohistochemical markers on lymph node biopsy between 1990 and 2020. Not all patients underwent skin biopsy for their rash, therefore we defined "suspected cutaneous AITL” as cases with documented rash occurring at the time of AITL diagnosis or during the disease course. A subset of cases were defined as "confirmed cutaneous AITL” if they had pathologist confirmed AITL on skin biopsy. Cutaneous presentations were excluded if another etiology, such as drug reaction or skin infection, was determined by clinical history and/or skin biopsy findings. We collected clinical data from patient medical records regarding patient demographics, disease characteristics, and clinical outcomes. The Chi-square test or Fisher's exact test was used to evaluate the association between two categorical variables. Wilcoxon rank sum test was used to evaluate the difference in a continuous variable between patient groups. Kaplan-Meier method was used for time-to-event analysis including progression free survival (PFS) and overall survival (OS). The Log-rank test was used to evaluate the difference in time-to-event endpoints between patient groups.
Results: Overall, 32% of the patients had suspected cutaneous AITL with various presentations, but most presented with a maculopapular rash (31%) on the legs (16%) that was pruritic (66%) with onset at about 4 months after the AITL diagnosis. Furthermore, 10% of all AITL patients had confirmed cutaneous AITL on skin biopsy, most commonly with a perivascular infiltrative pattern (69%).
The median WBC among patients with suspected cutaneous AITL was higher than AITL without skin findings (8.95 vs. 6.3; p-value=0.0036). Otherwise, there were no significant differences in clinical features for suspected or confirmed cutaneous AITL patients.
In terms of treatment response, patients without rash had a higher overall response rate (ORR) rate from the second line treatment compared to suspected cutaneous AITL patients (62.5% vs. 41.9%; p-value=0.049). Also, the rate of ORR from upfront treatment was higher among the patients with pruritus compared to the patients without pruritus (65.2% vs. 92.3%; p-value=0.0134).
The median OS time for all AITL patients was 35.3 months (95% CI: 31.1 ~ 47 months) with a 5-year OS of 36%. The median follow-up time was 53.5 months (95% CI: 44.1 ~ 64.6 months). There were no significant differences in OS for suspected cutaneous AITL or confirmed cutaneous AITL patients. The median PFS time was 12.8 months (95% CI: 10.4 ~ 17.5 months) with a 5-year PFS of 19%.
Conclusion: Our study corroborates the aggressive nature of AITL and its poor prognosis. AITL patients with pruritus may respond more favorably to upfront treatment, while AITL without skin involvement may respond better to second line treatment. However, we found no significant association between skin involvement and survival. Moreover, no histologic or immunophenotypic features in the skin were identified with prognostic value. Continued examination of disease characteristics for prognostic significance can serve to enhance the care for these patients.
Disclosures
Nair:Incyte Corporation: Honoraria. Huen:kyowa: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.