Abstract
Introduction The cytotoxic gamma delta T cells give rise to an extremely rare malignancy, known as Primary cutaneous Gamma-Delta T cell lymphoma (PCGDTCL), which represents < 1% of all lymphomas. These are considered aggressive lymphomas with a median survival of 15-31 months. Since they usually present as plaques in the extremities, they mimic nonspecific panniculitis and need a high index of suspicion for diagnosis. Using a large national cancer repository, the National Cancer Database (NCDB), we analyzed the demographic distribution, clinical characteristics, treatment strategies and survival outcomes and studied the impact of various factors on the survival of patients with PCGDTCL.
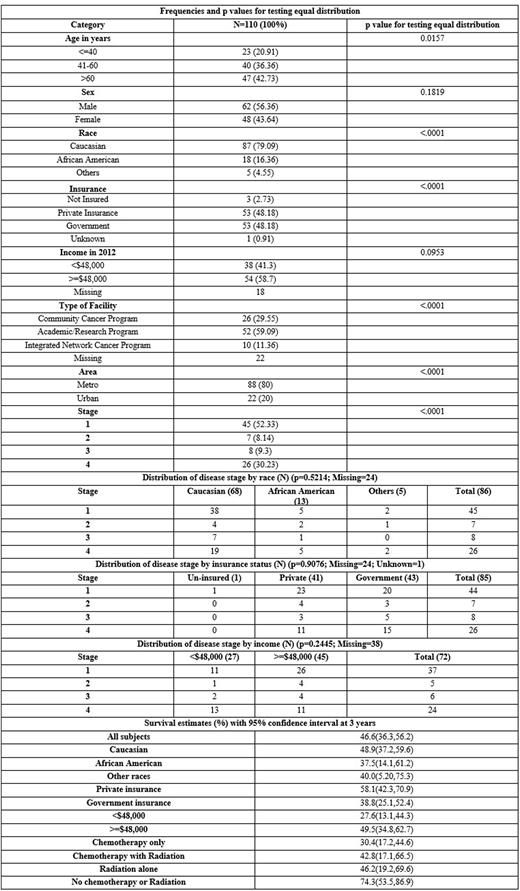
Methods The 2004-2018 NCDB file was used to extract patients with a diagnosis of PCGDTCL. We included patients who had skin and lymph nodes as the primary disease sites. All patients were adults aged ≥ 18 years. Frequencies and chi-square tests were used to compare patient distribution among various demographic and clinical characteristics as shown in the table. Kaplan-Meier (KM) analysis and hazard ratios (HR) were used to compare survival outcomes.
Results A total of 110 patients with PCGDTCL were identified. The table summarizes the distribution of patients by various demographic features and disease stage. The median age of our cohort was 58 years. Most of the patients were elderly males aged >60 years (>60 years: 42.73%, 41-60 years: 36.36%, <=40 years: 20.91%) (Males: 56.36%, Females: 43.64%). Caucasian race was the most common (Caucasian: 79.09%, African American: 16.36%). There was an equal distribution of patients using private and government insurance (48.18% each). Income, facility type, and area distribution is shown in the table. Most of the patients were diagnosed at stage 1 (52.33%), followed by stage 4 (30.23%). 55.88% (38/68) of Caucasians were diagnosed at stage 1 and 27.94% (19/68) were diagnosed at stage 4. Among African Americans, the distribution between stage 1 and stage 4 was 38.46% (5/13) each. On analyzing income categories, <$48,000 group had 48.15% stage 4 (13/27) and 40.74% (11/27) stage 1. Among the >=$48,000 group, 57.88% (26/45) were stage 1 and 24.14% (11/45) were stage 4. Distribution by insurance used is shown in the table. The distribution among various systemic treatment strategies used were as follows: Chemotherapy only - 47 (42.72%), Chemotherapy with Radiation - 17 (15.46%), Radiation alone -13 (11.82%), No chemotherapy or Radiation - 33 (30%). Among patients who did not receive chemotherapy or radiation, 79.17% had stage 1 disease.
Overall survival of the study group at 3 years was 46.6%. The group that did not receive chemotherapy or radiation had the highest 3-year survival (74.3%). Survival rates of the other treatment groups and the survival by race, income and insurance is represented in the table. HR estimates showed that compared to the no systemic therapy group, the chemotherapy [2.994 (95% CI 1.400, 6.401)p=0.0047] and chemotherapy with radiation [2.611 (95% CI 1.048,6.5090)p=0.0394] groups had more adverse outcomes. Comparison between the other treatment groups were not significant. The African American race had a lower overall survival (37.5%), but the HR did not reach significance compared to Caucasians [1.524 (95% CI 0.779,2.984)p=0.2187]. Having an income of <$48,000 had a lower survival (27.6%) with HR [2.151 (95% CI 1.225,3.778)p=0.0077] compared to the higher incomes. Government insurance had a lower survival (38.8%), but the HR did not show significance compared to private insurance [1.708 (95% CI=0.980, 0.977)p=0.0591].
Conclusion We provide one of the first descriptive analysis of a very rare lymphoma. Although the group that did not receive any chemotherapy or radiation had better survival, majority of the patients in this group were stage 1. We hypothesized that this group may have received topical treatments which may have not been captured in NCDB. Socioeconomic disparities significantly impact access to healthcare and is of particular importance in rare lymphomas like PCGDTCL. In our analysis, patients with a lower income had a worse survival. The survival was also lower among African Americans, although the HR was not significant. A higher percentage of African American patients and those with a lower income were also diagnosed at Stage 4. Limitations of our study include the use of non-population-based data and the confounding that may arise from it.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.