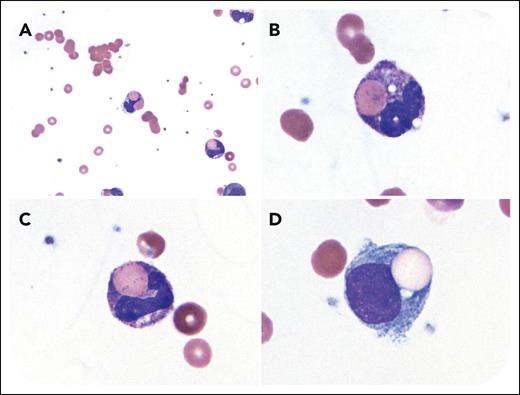
A 5-year-old girl presented with hematuria, jaundice, and lethargy. A week prior, she had a fever (100°F) and cough. Laboratory studies showed leukocytosis (leukocytes, 31 × 103/μL), normocytic anemia (hemoglobin, 4.9 g/dL), and evidence of intravascular hemolysis (total bilirubin, 13.8 mg/dL; lactate dehydrogenase, 2694 U/L; haptoglobin, <8 mg/dL). A direct antiglobulin test was positive for complement C3 and negative for immunoglobulin G (IgG). A peripheral smear revealed erythrocyte agglutination and erythrophagocytosis by neutrophils and monocytes (Wright-Giemsa stain; panel A original magnification ×600; panels B-D original magnification ×1000). A Donath-Landsteiner (DL) test was inconclusive owing to reactivity in the negative control, and antibody specificity studies were not performed. Mycoplasma pneumoniae immunoglobulin M was elevated, supporting recent infection. A diagnosis of paroxysmal cold hemoglobinuria (PCH) was rendered, and she received azithromycin and leukoreduced group O red blood cell (RBC) units. Over several days, her anemia began to resolve, and she was discharged home with follow-up.
PCH is an autoimmune hemolytic anemia caused by a cold-reactive complement-binding IgG antibody with specificity for the P blood group antigen, and M pneumoniae infection is a known trigger. Erythrophagocytosis by neutrophils is increasingly recognized as a feature of this disorder. The DL test can identify the biphasic hemolysin in PCH, and indirect testing using enzyme-treated reagent O RBCs and normal donor serum can increase diagnostic yield. Treatment typically involves RBC transfusions until brisk hemolysis resolves.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.