In this issue of Blood, Stachelscheid et al1 report a novel nuclear TCL1A-CDC20 axis that signals DNA damage-prone cell cycle transition and genomic instability, thereby accelerating aggressive chronic lymphocytic leukemia (CLL).
TCL1A is a proto-oncogene first identified in T-cell prolymphocytic leukemia. Upregulation of TCL1A via a gene rearrangement bringing TCL1 (on chromosome 14q31.2) under the influence of TCR (T-cell receptor) enhancer has been identified as a characteristic of the disease.2,3 The gene product is frequently overexpressed in many types of T- and B-cell lymphomas, and increased levels of TCL1A correlate with aggressive clinical behavior and poor prognosis in T- and B-cell lymphoma. Its expression is physiologically restricted to early developmental stage B and T cells and embryonic tissues.4 Genomic rearrangements or gain-of-function mutations involving the TCL1A locus are virtually absent in B-cell tumors.5,6 Accordingly, the molecular mechanism(s) and signaling pathway(s) by which TCL1A mediates oncogenicity in B-cell neoplasms are not well understood. Notably, transgenic mice expressing TCL1A in B cells (ie, Eμ-TCL1A or pEμ-B29TCL1A) develop CLL or germinal center–derived B-cell lymphoma, including Burkitt lymphoma (BL), follicular lymphoma (FL), and diffuse large B-cell lymphoma (DLBCL), suggesting unknown mechanism(s) and pathway(s) contributing to lymphomagenesis.7 Stachelscheid et al describe the pleiotropic effect of TCL1A as a major factor in the pathogenesis of CLL through acceleration of premature and DNA-damage–prone cell cycle transition causing aneuploidy, impaired DNA-damage repair, and increased cell survival signaling as well as apoptotic resistance.
The expression pattern of TCL1A, subcellular localization, and interactome may determine its physiological or tumorigenic properties. In this regard, the signaling consequences of subcellular site-specific TCL1A have not been fully explored. TCL1A encodes a 14 kDa nonenzymatic protein, which is functionally required to form homodimers that bind with AKT as a cofactor and enhances its kinase activity as well as promotes its nuclear transport.1,3 Constitutively active myristoylated AKT in murine B cells does not appear to recapitulate the oncogenic effect of TCL1A. Therefore, Stachelscheid et al investigated the role of the nuclear TCL1A in CLL pathogenesis. Because TCL1A itself does not have enzymatic activity or DNA-binding capability, it can be hypothesized that it forms multiprotein complexes to exert its effects.
Stachelscheid et al uses various proteogenomic approaches to identify the effectors and critical pathways perturbed by TCL1A to promote CLL growth. Further elegant and robust in silico, in vitro, and in vivo experimental approaches including multiple cell lines and transgenic murine models demonstrate that expression of TCL1A promotes premature and defective mitotic checkpoint protein complex composition by directly binding to CDC20. This disrupts the interaction of CDC20 with MAD2 and PLK1 in the spindle assembly checkpoint, leading to accelerated cell cycle transition and aneuploidy. The role of nuclear TCL1A and its effectors and pathways that are deregulated in lymphomagenesis are poorly understood. Stachelscheid et al demonstrate the signaling pathways (cell cycle transition, chromosomal segregation, DNA damage response, and apoptosis) affected and cell cycle modulators recruited by nuclear TCL1A to promote its oncogenicity. The study also demonstrates that the expression of nuclear localized TCL1A in an in vivo model promotes aggressive biologic behavior of CLL and significantly shorter survival compared with wild-type or membrane-targeted TCL1A.
Stachelscheid et al further show that in primary human CLL cells, high levels of TCL1A expression are inversely correlated with reduced levels of phospho-activated and cleaved ATM upon genotoxic stress. B cells from Eμ-TCL1A mice show reduction of p53 and accumulation of DNA double-strand breaks compared with wild-type control mice, suggesting that TCL1A promotes DNA damage and hinders the DNA repair response. However, the role of TCL1A in regulating DNA damage response needs further exploration to understand the mechanisms involved and assess the potential for therapeutic targeting.
Extensive genomic analyses of CLL published to date have not documented genomic lesions (mutations or copy number variations) of CDC20. However, bioinformatic analysis of publicly available databases by the authors demonstrates that transcript levels of CDC20 are significantly reduced in CLL compared with the levels in other B-cell neoplasms. They show that lower levels of TCL1A protein were observed in more aggressive CLL. Furthermore, low expression of CDC20 was directly proportional to high genomic instability. Downregulation of CDC20 in the Eμ-TCL1A CLL model further accelerated leukemic progression and increased aneuploidy.
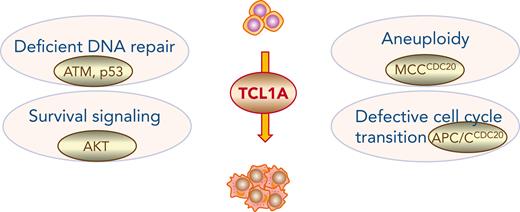
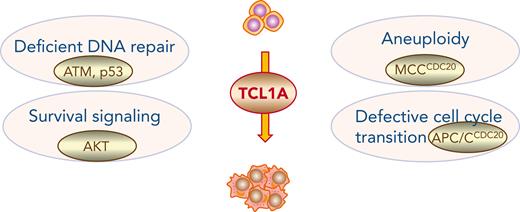
The role of TCL1A in impaired DNA damage repair pathway warrants further investigation. The results presented by Stachelscheid et al expand our understanding of the multifaceted mechanisms used by nuclear TCL1A to promote defective and accelerated cell cycle transition, aneuploidy, and impaired DNA damage response that collectively contribute to CLL pathogenesis (See figure). Considering the important insights offered by this investigation of TCL1A and its contribution to pathogenesis of CLL, it is important to identify whether similar mechanisms are used by TCL1A in other B-cell lymphomas such as BL, FL, and DLBCL. Furthermore, it is critical to determine the mechanisms involved in downregulation of CDC20 in aggressive CLL to exploit this avenue for therapeutic intervention.
Signaling pathways regulated by TCL1A in CLL. TCL1A functions as a pleiotropic adapter molecule regulating multiple signaling pathways (deficient DNA repair, increased survival, apoptotic resistance, aneuploidy, and defective cell cycle transition) resulting in genomic instability that contributes to pathogenesis of CLL. APC/C, anaphase-promoting complex; MMC, mitotic checkpoint complex.
Signaling pathways regulated by TCL1A in CLL. TCL1A functions as a pleiotropic adapter molecule regulating multiple signaling pathways (deficient DNA repair, increased survival, apoptotic resistance, aneuploidy, and defective cell cycle transition) resulting in genomic instability that contributes to pathogenesis of CLL. APC/C, anaphase-promoting complex; MMC, mitotic checkpoint complex.
Conflict-of-interest disclosure: The authors declare no competing financial interests.