Background:
Hemophagocytic lymphohistiocytosis (HLH) is a rare, under-diagnosed, potentially lethal condition marked by dysregulated hyperinflammation and widespread multi-organ dysfunction. There is currently no literature describing the differences in HLH outcomes according to its commonly reported risk factors. Therefore, authors of this study aimed to identify potential differences in the outcomes of HLH among various etiologies as well as update literature on the prevalence of risk factors for HLH in the United States.
Methods:
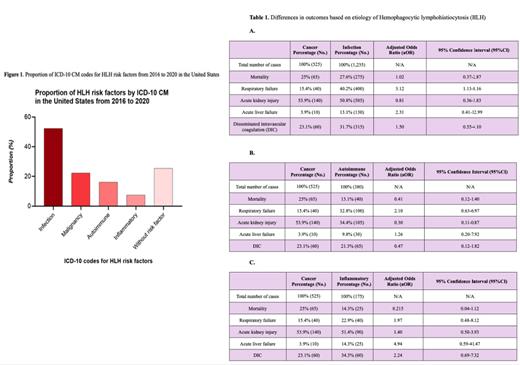
Using weighted data from the Nationwide Inpatient Sample (NIS) database from 2016 to 2020, we assessed prevalence of known HLH risk factors (infection, malignancy, auto-immune, and inflammatory syndromes) and HLH outcomes (mortality, length of hospital stay, total healthcare charges, complications) stratified by HLH etiology (infection, malignancy, auto-immune, inflammatory). Baseline characteristics were analyzed using T-test for continuous variables and Chi-Square for categorical variables, and a multivariate regression analysis was used to estimate outcomes between races. Data analysis was performed using STATA® Version 17.0/SE Software, with statistical significance set at p < 0.05.
Results:
Among a total of 2,685 individuals admitted with a primary diagnosis of HLH, 52% (N=1,350) had an infection (27% bacterial, 28% viral,14% fungal, and 1% parasitic), 22% were with malignancy (N=525)(14% lymphoma, 2% leukemia, 3% plasma cell proliferation, 3% myeloproliferative disease, and 4% solid tumors), 16% had a history of autoimmune disease (N=380), and 7% had an inflammatory syndrome (N=175). 25% had no ICD-10 codes for common risk factors of HLH.
Among patients with HLH and autoimmune disease, we noted a predominance of females (77%, p<0.001). Individuals with HLH and cancer had more comorbid conditions (Charlson index: 3 in 58%, p<0.001). Pertaining to outcomes, when compared to those with cancer, individuals with infection had a 3-fold increase in respiratory failure (adjusted Odds Ratio (aOR)=3.12, 95%CI: 1.13-8.61), while those with autoimmune disease had reduced odds of acute kidney injury (aOR=0.30, 95%CI: 0.10-0.87). There were no significant differences in the length of hospital stay, the total healthcare expenditures, mortality and the other complications (cardiac arrest, acute kidney injury, respiratory failure, disseminated intravascular coagulation, and acute liver failure) among HLH secondary to cancer versus other risk factors.
Discussion:
Our study findings demonstrate that infection is the most common trigger for secondary HLH in the U.S., followed by malignancy. This is consistent with existing literature. Individuals who develop HLH associated with the infection have a 3-fold higher odds of acute respiratory failure compared to those with HLH resulting from other cancer. This warrants increased vigilance, and the potential need for a lower threshold for mechanical ventilation to mitigate adverse outcomes in patients with HLH secondary to infection.
Disclosures
No relevant conflicts of interest to declare.