Introduction: It is estimated that approximately 3.5 million active duty service members (ADSM) have deployed to Afghanistan and Iraq from 2001-2022. There has been concern about potential exposure to carcinogenic or environmental hazards during overseas deployment. A recent study found ADSM with no prior deployments had an increased risk of cancer mortality compared to those who had served in Operation Iraqi Freedom/Operation Enduring Freedom. Moreover, Nordic personnel with military deployments were also found to have a lower risk of cancer related death when compared to the general population. While there may be a link between potential environmental exposures, there is a lack of data on non-Hodgkin lymphoma (NHL) survival in servicemembers who have previously deployed. Additionally, there are no studies comparing risk of aggressive B-cell lymphoma in these patient populations.
Methods: Documented cases of NHL in the DoD's Tumor Registry (Oncolog) from 2001-2022 were obtained. This information was compared to the Defense Manpower Data Center's deployment data and the two datasets were merged. ADSMs and retirees were included; dependents were excluded. A multivariable logistic regression analysis was done to assess the impact of prior deployment on cancer survival in NHL, accounting for age, race, cancer stage, ethnicity, and gender.
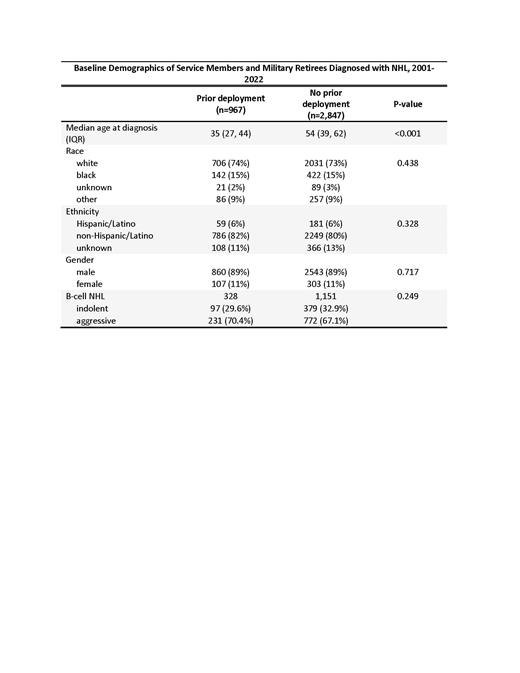
Results: There were 2,295 servicemembers and retirees diagnosed with NHL from 2001-2022. About 20% had previously deployed (n=467). Median age at diagnosis in those who had deployed was 35 years compared to 54 years for non-deployed (p<0.001). Race, ethnicity, and gender were similar between both arms. Multivariable logistic regression analysis demonstrated prior deployment was associated with better survival after accounting for age, race, stage, ethnicity, and gender (OR 0.63, 95% CI 0.40-0.97, p=0.037). In addition to deployment status, other variables that influenced survival were age (OR 1.04, 95% CI 1.03-1.54, p<0.001), stage (OR 2.92 for stage IV vs. stage I, 95% CI 2.06-4.15, p<0.001), and race (OR 1.97 for black vs. white race, 95% CI 1.37-2.83, p<0.001). To assess whether NHL subtype played a role in these findings, a post-hoc analysis was performed on patients with B-cell NHLs, revealing that ADSM with prior deployment were equally likely to have indolent and aggressive subtypes of B-cell NHL as ADSM who had never deployed. Among personnel with prior deployment, 29.6% and 70.4% had indolent and aggressive B-cell NHLs respectively, compared to 32.9% and 67.1% amongst those who never deployed (p=0.25).
Conclusions: Military personnel with NHL who had previously deployed lived longer than those with no prior deployment, even after adjusting for age differences between the two cohorts. These findings are not attributable to B-cell NHL subtype (i.e. deployed personnel did not have more indolent NHLs than non-deployed personnel). These results highlight the healthy deployer effect, in which ADSM who are deployable are required to meet minimum fitness standards, undergo a physical health assessment, and do not have disqualifying comorbidities. This study did not evaluate whether an overseas deployment is associated with an increased risk of NHL, but it does appear to provide evidence that potential deployment-related exposures do not appear to alter the biology or subtype of B-cell NHLs.
Disclaimer: The contents of this publication are the sole responsibility of the author(s) and do not necessarily reflect the views, opinions or policies of the Department of Defense (DoD) or the Departments of the Army, Navy, or Air Force. Mention of trade names, commercial products, or organizations does not imply endorsement by the U.S. Government.
Disclosures
Morris:Janssen: Speakers Bureau.