Background
Pediatric-inspired regimen have remarkably improved the prognosis of adult ALL, particularly for adolescent and young adult (AYA) patients. The role of allo-HSCT was controversy in the era of pediatric-inspired regimen. Some study revealed that patients treated with pediatric-inspired regimen those who achieved MRD negative may not require allo-HSCT (Ref1. Ribera et.al, Blood 2021; Ref2. Dhedin et.al, Blood, 2015). To address this issue, we performed study on HR ALL population in pediatric-inspired PDT-ALL-2016 cohort, by comparing outcome of allo-HSCT and chemotherapy groups.
Methods
PDT-ALL-2016 cohort is a GRAALL-backbone pediatric-inspired regimen (NCT03564470), patients diagnosed with ALL in Nanfang hospital were enrolled in JAN-2016 to DEC-2021. High-risk features included: WBC higher than 30×10^9/L for B-ALL or 100×10^9/L for T-ALL; pro-B or ETP; presence of t(9;22), t(1;19), t(4;11) or 11q23 rearrangements, Ph-like, complex karyotype, hypodiploid or near triploid; IKZF1 deletion/muation. Patients diagnosed with HR-ALL and achieved CR1 after induction were enrolled in this study. The left-truncated Kaplan-Meier estimator was used to compare the overall survival (OS), event-free survival (EFS), cumulative incidence of relapse (CIR) and non-relapse mortality (NRM).
Results
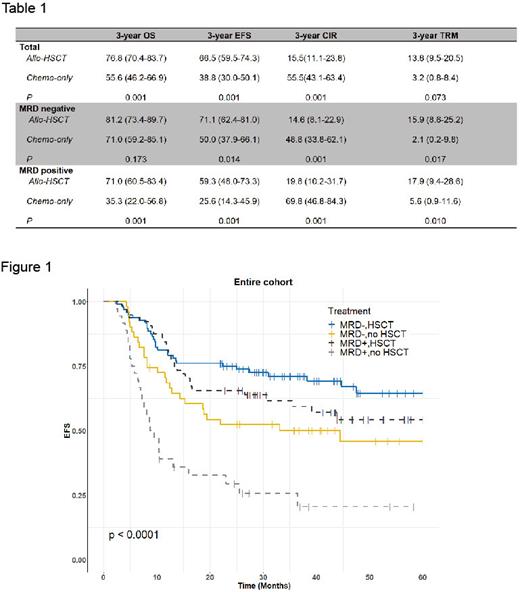
A total of 265 HR-ALL patients were enrolled in this study, 168 patients in allo-HSCT and 97 patients in chemotherapy cohorts, respectively. The baseline characteristics between two cohorts were comparable. With a median follow-up time of 43.6 months (3.8-60.0 months), the 3-yr OS and EFS were better in allo-HSCT cohort compared with chemo-only cohort (3-yr OS, 76.8% VS 55.6%, P<0.001; 3-yr EFS, 66.5% VS 38.8%, P<0.001). Meanwhile, the allo-HSCT cohort had lower CIR and higher but acceptable NRM compared with chemo-only cohort (3-yr CIR, 15.5% VS 55.5%, P<0.001; 3-yr NRM, 13.8% VS 3.2%, P<0.001; Table 1).
For MRD positive subgroup (allo-HSCT, n=64; chemo-only, n=37), patients who underwent allo-HSCT had longer EFS and OS, and lower CIR compared with chemo-only cohort (3-yr OS, 71.0% VS 35.3%, P<0.001; 3-yr EFS, 59.3% VS 25.6%, P<0.001; 3-yr CIR, 19.8% VS 69.8%, P<0.001).
Of note, for MRD negative subgroup (allo-HSCT, n=96; chemo-only, n=51), the allo-HSCT cohort had longer EFS and lower CIR compared with chemo-only cohort, the OS also improved by allo-HSCT (3-yr OS, 81.2% VS 71.0%, P=0.173; 3-yr EFS, 71.1% VS 50.0%, P=0.014; 3-yr CIR, 14.6% VS 48.8%, P<0.001; Fig 1).
In multivariable analyses, allo-HSCT was protective factors for OS (HR=0.37), EFS (HR=0.56) and CIR (HR=0.45), and negatively infected NRM (HR=4.66).
Conclusion
Here, we showed that allo-HSCT further improved the outcome of HR ALL regardless of the MRD status, in the era of pediatric-inspired regimen. The survival advantage of allo-HSCT came from lower CIR compared with chemotherapy only.
Furthermore, compared with published data, the NRM was more acceptable in our cohort. It is the high NRM (20-40%) in other studies ( Ref1. Ribera et.al, Blood 2021; Ref2. Dhedin et.al, Blood, 2015; Ref3. Wieduwilt et.al, leukemia, 2021; Ref4. Seftel et.al, AJH, 2015) that counterbalanced the benefit of CIR by allo-HSCT, which highlight the importance of experienced management for total therapy in adult ALL.
This research was supported by the National Natural Science Foundation of China(NFSC82170163, 81970147), Clinical Study of Nanfang Hospital(LC2016ZD009/2019CR012).
Disclosures
No relevant conflicts of interest to declare.