Proteasome inhibitors are clinically approved and highly effective for treating multiple myeloma in the first line setting, but exhibit little effectiveness for treatment of other hematological malignancies. In this study, we set out to determine why acute myeloid leukemia (AML) is largely refractory to proteasome inhibition and to determine if we could sensitize human AML to this class of therapeutics.
Efficacy of proteasome inhibitors in multiple myeloma partly depends on disruption of protein homeostasis (proteostasis). This is driven by an accumulation of misfolded proteins that overwhelm the endoplasmic reticulum and activate the unfolded protein response (UPR) - part of the integrated stress response (ISR) pathway. Due to their highly secretory nature, myeloma cells exhibit relatively elevated baseline endoplasmic reticulum stress, and are thus preferentially sensitive to proteasome inhibition as they readily activate a terminal ISR. We hypothesized that AML cells are better able to cope with proteasome inhibition by activating alternative stress response pathways that rebalance proteostasis.
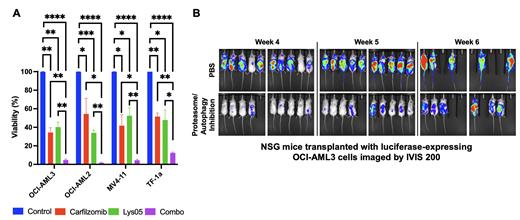
We determined that proteasome inhibition fails to significantly disrupt proteostasis in human AML cells. Instead, RNA-sequencing studies suggested that AML cells respond to proteasome inhibition by activating at least two distinct stress response pathways, including autophagy - a key pathway utilized by normal hematopoietic stem cells to preserve proteostasis. Using a GFP-LC3-RFP fluorescent reporter system, we found that proteasome inhibition significantly increased autophagic flux in multiple human AML cell lines in a dose-dependent manner. Dual, concurrent pharmacological proteasome and autophagy inhibition was required to disrupt proteostasis across multiple human AML cell lines, as it resulted in a profound accumulation of unfolded protein. Proteostasis disruption caused by concurrent proteasome and autophagy inhibiton resulted in activation of a terminal ISR response in AML cells, marked by activation of eIF2a signaling and its downstream effectors ATF4 and CHOP. Consistent with this activation, dual proteasome and autophagy inhibition dramatically attenuated protein synthesis and synergistically reduced viability in multiple human AML cell lines (Figure 1A, * P<0.05, ** P<0.01, *** P<0.001, **** P<0.0001). In addition, dual proteasome and autophagy inhibition reduced proliferation and induced massive apoptosis in these human AML cell lines and in primary AML patient samples. Surprisingly, this activity was not driven by the canonical PERK ( EIF2AK3)-mediated endoplasmic reticulum UPR, but was instead driven by an alternative eIF2a kinase PKR ( EIF2AK2). Treatment with a small molecule inhibitor to PERK had no significant effect on apoptosis while an inhibitor to PKR partially rescued the increased apoptosis and decreased protein synthesis induced by dual proteasome and autophagy inhibition. This suggests that the proteostasis network is uniquely remodeled in AML. Furthermore, in contrast to AML cells, dual proteasome and autophagy inhibition was well tolerated by healthy human CD34+ hematopoietic stem and progenitor cells, suggesting a tractable therapeutic window for treating AML. Indeed, dual proteasome and autophagy inhibition was tolerated in vivo, and decreased leukemia burden in mice xenografted with human AML cell lines (Figure 1B).
Overall, this study revealed that AML cells rewire the proteostasis network to promote growth, survival, and therapeutic resistance. Targeting the unique configuration of the proteostasis network is uncovering new therapeutic strategies to eliminate AML.
Disclosures
No relevant conflicts of interest to declare.