Introduction:
Myelodysplasia-related gene mutations have been newly included as diagnostic criteria for acute myeloid leukemia, myelodysplasia-related (AML-MR) in the new 5th World Health Organization (WHO) classification. Myelodysplasia-related gene mutations are defined as somatic mutations of eight genes - SRSF2, SF3B1, U2AF1, ZRSR2, ASXL1, EZH2, BCOR, and STAG2. According to the new classification, some cases diagnosed as AML, not otherwise specified (NOS), which has no prognostic significance, can be revised as AML-MR, which has poor prognosis regardless of variant allele frequency (VAF) of myelodysplasia-related gene mutations. The prognostic impact of VAF of myelodysplasia-related gene mutations in the patients newly diagnosed as AML-MR is not well established. In this study, we evaluated the proportion of the patients who were formerly diagnosed as AML, NOS and can be newly diagnosed as AML-MR according to the new classification, and the prognostic impact of VAF of myelodysplasia-related gene mutations.
Methods:
From March 2019 to February 2023, we retrospectively reviewed the medical records of the patients newly diagnosed as AML, NOS according to the revised 4th edition of WHO classification. We also reviewed the results of mutation profiles detected by next generation sequencing for identifying myelodysplasia-related gene mutations. The limit of detection for each variant was VAF 2%. We categorized patients into two groups; AML, NOS with myelodysplasia-related gene mutations (AML, NOS, MR+) group who can be newly diagnosed as AML-MR according to the new classification and AML, NOS without myelodysplasia-related gene mutations (AML, NOS, MR-) group. For comparing the survival rates between two groups, we performed Kaplan-Meier curve analysis. We also classified AML, NOS, MR+ group according to the VAF; 2-10% and ≥10% of somatic mutations and compared the survival rate.
Results:
We reviewed 98 patients newly diagnosed as AML, NOS. Among them, 55.1%(54/98) of patients had myelodysplasia-related gene mutations. The distribution of myelodysplasia-related gene mutations in these patients were as follows; ASXL1 (50.0%, 27/54), U2AF1 (29.6%, 16/54), BCOR (25.9%, 14/54), SRSF2 (25.9%, 14/54), STAG2 (13.0%, 7/54), SF3B1 (9.3% 5/54), EZH2 (7.4%, 4/54), and ZRSR2 (3.7%, 2/54). The diagnosis of these patients can be revised as AML-MR according to the new classification. Among these patients, variants of myelodysplasia-related gene mutations with VAF 2-10% and ≥10% were detected in 7 and 47 patients, respectively.
The survival rate of AML, NOS, MR+ group (2 year survival rate, 32.0%) was inferior than that of AML, NOS, MR- group (3 year survival rate 44.6%), although the difference was not statistically significant ( p=0.069).
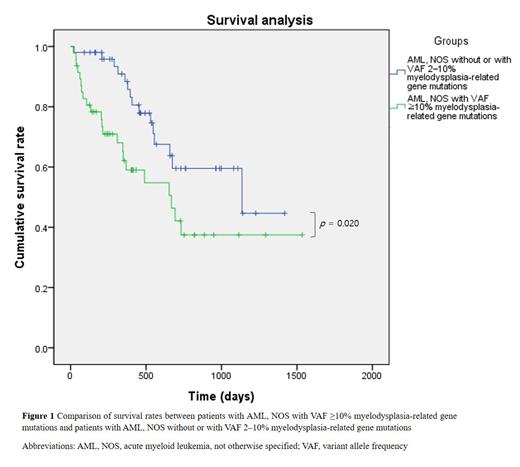
Considering VAF of somatic mutations, the survival rate of patients with AML, NOS with VAF ≥10% myelodysplasia-related gene mutations (N=47) was significantly inferior than that of patients with AML, NOS without or with VAF 2-10% myelodysplasia-related gene mutations (N=51) ( p=0.020) (Figure 1).
Conclusions:
More than half of the patients formerly diagnosed as AML, NOS can be re-diagnosed as AML-MR according to the 5th WHO classification. More than 10% of VAF of myelodysplasia-related gene mutations can be associated with worse survival rate among patients newly diagnosed as AML-MR. These results suggest that VAF of myelodysplasia-related gene mutations has prognostic impact and should be considered when predicting survival rate.
Disclosures
No relevant conflicts of interest to declare.