Background: Obesity and hormonal contraception (HC) are independent risk factors for venous thromboembolism (VTE). Thirty eight percent of women in the United States (US) are obese, and the prevalence of childhood obesity in the US is among the highest in the world. Obesity (BMI>30 kg/m2), increases VTE risk via several mechanisms, and the VTE risk in obese individuals is 2.5 times higher than that of their non-obese peers. More than half of women aged 15-49 years use some form of contraception, and 14% report using oral contraceptive pills specifically. The overall VTE risk with combined hormonal contraception (CHC) is approximately two-fold higher than an individual's baseline risk, with further increase depending on the type/dose of progesterone and estrogen, and route of administration.
To date case-control and cohort studies have demonstrated an increased VTE risk among obese contraceptive users. But these data do not include adolescents and were derived from populations with relatively low rates of obesity.
This study aimed to assess and compare the VTE risk among obese females, age 10-44 years, who were prescribed HC compared to non-obese HC users and obese non-users utilizing a national electronic-medical record database. Using a large national database allowed the inclusion of females from diverse ethnic, economic, and geographic background.
Methods: Population level data was collected from TriNETX, LLC, an administrative database that contains comprehensive inpatient and outpatient data from 56 tertiary care hospitals in US. Prevalence data regarding the type and dose of progesterone and estrogen and mode of administration was assessed.
Data on females ages 10-44 years from 1/1/2000 to 12/30/2022, who received a new prescription for any HC as identified by the prescription name in pharmaceutical claims and procedure codes was analyzed. Recorded BMI was used to divide the cohort into obese and non-obese individuals as per CDC guidelines. VTE events were defined as presence of ≥1 ICD 9 or 10 codes for VTE diagnosis and presence of a prescription for an anticoagulant drug within the first year after hormonal prescription. Data was summarized descriptively and VTE rates were calculated.
Results: Of the 97,026,002 females who met inclusion criteria, 1,370,481 were obese and 2,649,987 were non-obese. The overall rate of VTE for obese vs. non-obese users was 0.9% vs. 0.5% (p<-0.001) and obese HC users vs. obese non-users was 0.9 and 1.06% (p<0.05).
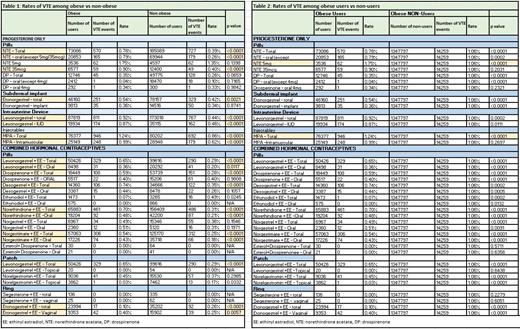
VTE rates among obese users versus non-obese users was significantly higher for most progesterone only options (p<0.001), excluding drospirenone only pills and high dose norethindrone (Table 1). A similar pattern of higher VTE rates in obese vs non-obese users was observed for the majority of CHC preparations with few exceptions (p<0.001). (Table 1)
In general, VTE rates were higher among obese non-users compared to obese users. However, the rate of VTE was significantly higher among obese users of oral norethindrone 5mg and all medroxyprogesterone acetate users (p<0.001). (Table 2)
Discussion: Utilizing the data from a large inpatient/outpatient administrative database, our study shows that obese HC users have a higher VTE rate within one year of initiating HC when compared to non-obese HC users, for progesterone only options (excluding drospirenone, high dose norethindrone) and most CHCs.
With few exceptions, obese HC non-users had a higher rate of VTE when compared to obese users. This observation is likely due to confounding by indication bias as prescribers may avoid HC in individuals with underlying risk factors for VTE. Applying propensity score analysis and examining different subcategories of obesity may help overcome this bias in future analysis.
Our study highlights the utility of large databases to study healthcare outcomes of VTE risk in females with and without obesity and HC users and non-users. Although limited by the use of administrative claims data and acknowledging that all statistically significant results may not be clinically significant, our study suggests obesity as a VTE risk factor in females for most HCs.
Disclosures
Rosovsky:Pulmonary Embolism Response Team: Membership on an entity's Board of Directors or advisory committees, Other: President-Elect; BMS: Consultancy; Dova: Consultancy; Janssen: Consultancy, Other: Research funding is to my institution, Research Funding; Abbott: Consultancy; Penumbra: Consultancy, Other: National Lead Investigator for STORM PE; Inari: Consultancy.