Introduction
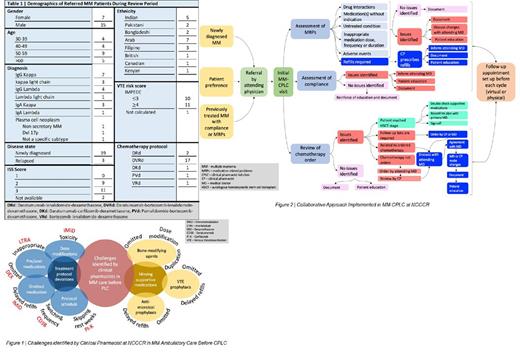
Multiple Myeloma (MM) is a chronic and incurable hematologic malignancy affecting the plasma cells, and is more prevalent among the elderly. Interprofessional patient care showed superiority over physician-only care in multiple settings, including MM. (Sweiss K et al.2019)In Qatar, real-world data analysis of MM patients treated in the ambulatory setting at the National Center for Cancer Care and Research (NCCCR) showed that clinical pharmacists (CPs) had an evident role in therapy optimization and ensuring adherence to treatment protocol schedule and supportive medications.(Elazzazy S et al.,2023) We aimed to provide a more structured and accessible link to MM patients considering the complexity of their treatment protocols and supportive care through the establishment of a clinical pharmacist-led clinic (CPLC). The most common challenges to optimum care of MM patients in the NCCCR before CPLC were identified and categorized (Figure 1) and then used to design the collaborative model for the MM CPLC (Figure 2).
Methods
The collaborative MM CPLC was initiated at NCCCR in February 2022. A collaborative practice agreement was established for this clinic, to allow clinical pharmacists -managing MM patients- to issue refills for supportive medications, and order any necessary laboratory tests. To investigate the quality of care provided by the clinic, data was retrospectively collected and analyzed for all MM patients managed in the clinic between February 2022 and February 2023. All patients who were newly diagnosed with MM were eligible for referral by the attending physician. Dedicated advanced hematology CPs provided consultation twice weekly for referred patients without additional fees. The provided services (in-person or virtual) included thorough medication profile review (prescribed antineoplastic and refills of supportive medications), and ordering follow-up laboratory tests. Services also included assessment and optimization of medication adherence, including immunomodulators and supportive medications (i.e., Venous Thromboembolism (VTE) prophylaxis, antimicrobial prophylaxis, bone modifying agents and vaccinations), providing comprehensive patient education, and communicating the recommended adjustments with physicians.
Results
During the 12-month period, there was a total of 22 patients referred to the clinic. The average age for patients was 51 years (range 36-72). Patient characteristics are summarized in Table 1. The total number of documented encounters with the pharmacists was 73 visits, corresponding to a median of 4 visits per patient (range 1-11). The total amount of time spent with each patient over the course of their referral was 15 minutes. A total of 343 CPs interventions (average of 5 interventions per visit) were performed with an acceptance rate of 100%. The most common intervention was medication reconciliation (n=124), followed by monitoring for medication outcomes (n=72, safety and efficacy), addition of required medication (n=40), patient education (n=27), issuing refills (n=24), drug interactions review and management (n=19), suggesting referrals to relevant subspecialities (n=16), identification of adverse drug reactions (n=7), and required dose adjustments (n=12). Twenty-two medication refills for supportive medications and eight pre-chemotherapy laboratory investigations were issued and ordered by CPs, respectively. All newly diagnosed patients were started on the appropriate bisphosphonate therapy without the previously observed delay, with the median from diagnosis to initiation being 14 days [range from 1 to 117 days]. All clinic patients were maintained on the appropriate VTE prophylaxis (aspirin [n=14], rivaroxaban [n=7], warfarin [n=1]). All patients were adherent to antiviral and Pneumocystis jirovecii Pneumonia prophylaxis.
Conclusion
CPLC for MM patients treated in the ambulatory setting provided a robust and timely link to patients in alignment with the published literature. The newly implemented collaborative prescribing model in MM clinic encouraged the expansion of pharmacy services in other ambulatory clinics. Our collaborative model could be potentially applied to different cancer settings to optimize a safe and effective patient care. Further analysis is planned to compare the adherence to international MM care guidelines pre- and post-launch of our CPLC.
Disclosures
No relevant conflicts of interest to declare.