Introduction: Acute lymphoblastic leukemia (ALL) in the pediatric population has a 5-year overall survival that exceeds 90%, however, the survival rate drops significantly in the adolescent and young adult (AYA) population. Notably, the AYA contribute to 80% of ALL mortality despite representing less than one-fourth of total ALL cases. The challenges related to caring for adolescents and young adults with malignancies have become increasingly well recognized and the impacts of racial, socioeconomic, and psychosocial disparities as potential contributors to AYA ALL survival rates are only recently being characterized.
Methods: We conducted a retrospective cohort study using the Nationwide Inpatient Sample (NIS), the largest all‐payer database of hospital admissions in the United States, from January 1, 2011 through December 31, 2020. The study sample consisted of AYA patients 15-39 years of age, as defined by the National Cancer Institute. ALL-related hospitalizations were captured using ICD-9 and 10 codes indicative of ALL. We performed temporal trends analysis to assess inpatient death among ALL hospitalizations by race/ethnicity using joinpoint regression. We used adjusted survey logistic regression analyses to assess associations between race/ethnicity and in-hospital mortality among ALL hospitalizations.
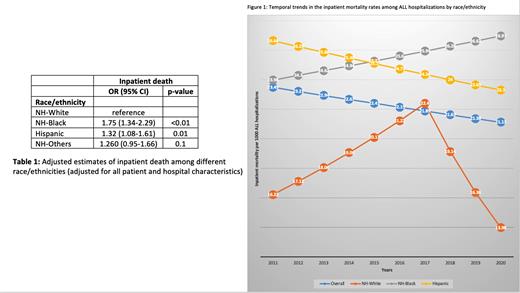
Results: Our data captured 138,923 ALL-related hospital encounters of AYA patients from 2011 to 2020. In our cohort, 73.1% of ALL hospitalizations were in patients younger than 30, and 26.9% were in patients between the ages of 30 and 39. AYA NH-Black patients with ALL had twice the odds of inpatient mortality as compared to NH-White patients [odds ratio (OR), 95% confidence interval: 1.75 (1.34-2.29)] (Table 1). While the rate of inpatient mortality improved in the overall AYA population over our 10-year study period, strikingly, the rate of inpatient mortality instead increased in NH-Black patients (Figure 1). In contrast, NH-White patients saw the lowest rate of inpatient mortality, both at the start and at the end of our study period (Figure 1). Although the inpatient mortality rate in Hispanic patients improved over time, these patients remained at an increased likelihood of inpatient mortality compared to their NH-White counterparts [OR 1.32 (1.08-1.61)] (Table 1).
Conclusion: Survival gains in the AYA population have improved only modestly compared to that of their pediatric and adult counterparts, and here we report that these survival gains are even further stratified and disparate depending on patient race/ethnicity with worse outcomes in NH-Black patients. It is important to better understand the disparities that impact the AYA population, which is particularly vulnerable to social factors impacting their care. Study limitations include lack of data pertaining to treatment received, including pediatric versus adult treatment protocol or bone marrow transplant status. Disparate access to centers of excellence, stem cell transplant and blinatumomab may certainly be contributors to the disparate outcomes described herein.
Disclosures
No relevant conflicts of interest to declare.