Background:
Sickle Cell Disease (SCD) patients are predisposed to several SCD related complications such as vasocclusive crisis, asplenia, haemolytic crisis and bacterial infection. Despite several other complications encountered by SCD patients during the first few years of life, invasive bacterial infections caused by Streptococcus pneumoniae, Haemophilus influenzae type b, and non-typhi Salmonella species have been reported to be the predominant cause of morbidity and mortality in sickle cell disease patients in many countries (Williams et al. 2009). This is because most SCD patients develop functional asplenism in their early years of life because of repeated episodes of sickling-induced splenic infarction which predisposes them to episodes of infections caused by encapsulated bacteria such as such as Streptococcus Pneumoniae, Haemophilus influenzae type b, and non-typhoidal Salmonella species. The two major prophylactic interventions are vaccination, and daily oral penicillin at least until the fifth year to protect the SCD populations from encapsulated bacterial infections.
Aims
The aim of this study was to determine the prevalence of invasive bacterial infections and their antimicrobial resistance patterns in SCD patients admitted at the Medical Research Council the Gambia (MRCG) Ward in the era of Pneumococcal Conjugate Vaccine and Haemophilus Influenzae b vaccination in the Gambia.
Methods and Results
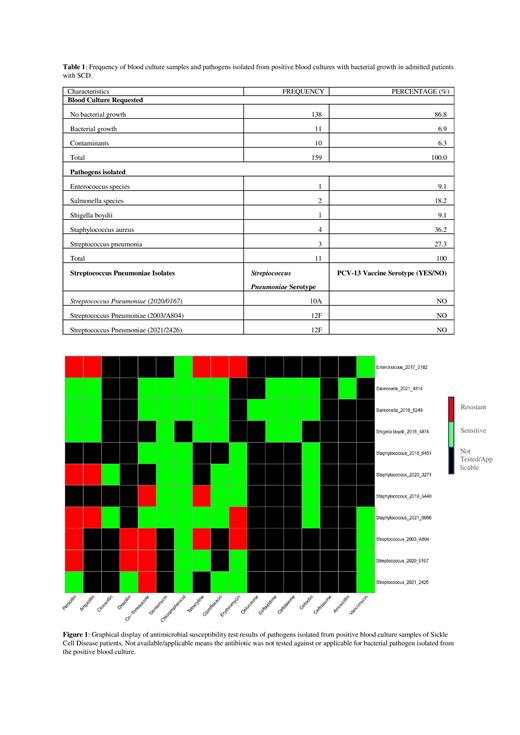
This study was conducted in the clinical laboratory department of MRCG. We retrospectively generated haematological, and blood culture data from our electronic medical records from 2015 to 2022 of SCD patients admitted to MRCG Ward. Of 380 SCD patients, blood culture was requested for 159. Of the 159 admitted SCD, 11 patients had qualified positive blood cultures. Five different types of pathogens were isolated from these positive blood cultures: 4 Staphylococcus aureus, 3 Streptococcus pneumoniae, 2 Salmonella species, 1 Enterococcus species, and 1 Shigella boydii. No episode of bacteremia caused by Haemophilus influenzae type b was identified. The molecular serotyping of the Streptococcus pneumoniae isolates revealed non-vaccine serotypes 10A, 12F and 12F. From our AST result, two of the three Streptococcus pneumoniae were resistant to penicillin antibiotics. The Staphylococcus aureus isolates were penicillin resistant but cefoxitin sensitive, hence no methicillin (oxacillin) resistant Staphylococcus aureus was reported., Generally, the isolated pathogens were all sensitive to chloramphenicol, and vancomycin.
Conclusion:Streptococcus pneumoniae and Staphylococcus aureus were the most common cause of bacteremia in these admitted SCD patients. The presence of non-typhoidal Salmonella and Shigella infection coupled with penicillin resistance should be considered during penicillin prophylaxis and empirical treatment regimens for SCD patients and future SCD management policies in the Gambia.
Disclosures
No relevant conflicts of interest to declare.