Background
Cardiovascular complications, especially pulmonary hypertension, are a known cause of mortality in patients with sickle cell disease (SCD). With advances in medicine and the introduction of various disease-modifying medications, the incidence and prevalence of cardiovascular complications are poorly documented.
Aim
To determine rates of cardiovascular complications in patients with SCD in the modern era of disease-modifying medications in a single center.
Method
We performed a retrospective observational single-center study of patients with SCD: all genotyped and ≥16 years old who had a recent echocardiogram performed during the study period of 2019-2023. Demographics, echocardiogram results, and laboratory findings were collected and analyzed. Descriptive statistics are presented in percentages, medians, and interquartile ranges. An unpaired Student's t-test and Fisher's exact test were used to determine, where appropriate, the level of significant differences among continuous and categorical variables, respectively, with p value <0.05 considered statistically significant. Data was analyzed using GraphPad Prism version 9.0.2.
Results
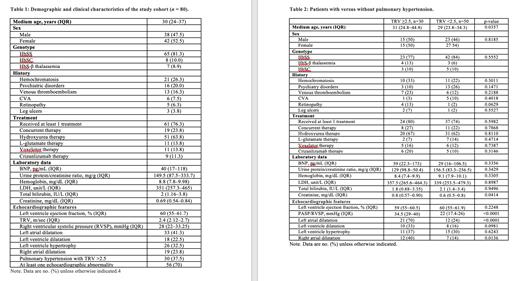
As of June 2023, 80 patients (38 male and 42 female, median age 30 years) had undergone a routine transthoracic echocardiogram. Sixty-five patients had the HbSS genotype, 8 HbSC, and 7 HbSB null. Sixty-one patients had received at least one treatment, and 19 (24%) were on concurrent therapy. Hydroxyurea was the common SCD-modifying therapy that the patients received (51 patients), followed by L-glutamine and voxelotor (11 each) and crizanlizumab (9 patients).
In total, 56 (70%) patients had at least one cardiac abnormality. The most common cardiac abnormality was left atrial dilatation (41%), followed by left ventricular hypertrophy (33%), right atrial dilation (24%), and left ventricular dilatation (23%). Pulmonary hypertension was present in 30 (38%) patients with tricuspid regurgitation velocity (TRV) ≥2.5 msec (Table 1).
The cohort of patients with pulmonary hypertension tended to be older (median age 31 years, p=0.0357), have a higher creatinine level (median 0.8, p=0.0414), and have coexisting echocardiographic abnormalities such as left atrial dilatation (70% vs. 24%, p<0.0001) or right atrial dilatation (40% vs. 14%, p=0.0136) than SCD patients without pulmonary hypertension (Table 2).
Conclusion
We present a comprehensive echocardiographic assessment of patients with SCD. Despite advances in the treatment of SCD, there remains a high prevalence of cardiac involvement in SCD patients. We found out that 70% of the patients we reviewed had at least one cardiac abnormality on echocardiography. Left atrial dilatation and left ventricular hypertrophy were the most common cardiac abnormalities noted. Pulmonary hypertension was observed in 37.5% of patients with co-existing right and left atrial enlargement. Larger studies are needed to corroborate these findings.
Disclosures
Idowu:Global Blood Therapeutics: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Forma Therapeutics: Research Funding; Novartis: Consultancy, Research Funding; Novo Nordisk: Consultancy, Research Funding; Bluebird Bio: Consultancy; Pfizer: Consultancy, Research Funding, Speakers Bureau; Alexion: Research Funding; Vertex: Consultancy; Agios Pharmaceuticals, Inc.: Research Funding.