Introduction:
Bleeding manifestations in patients with immune thrombocytopenia (ITP) range from mild skin bruises to lifethreatening intracranial hemorrhage. When the risk of bleeding is becoming high or life-threatening bleeding events occurs, we often use a combination of therapies to rapidly raise platelets to the safe range, including platelet transfusions, high-dose glucocorticoid, and intravenous immunoglobulins. Recombinant human thrombopoietin (rh-TPO) and thrombopoietin receptor agonists (TPO-Ra) are two kinds of thrombopoietic drugs commonly used in China. In patients with severe ITP refractory to glucocorticoids, we lack experience with the use of rh-TPO and TPO-Ra in this emergency situation.
Patients and methods:
We included ITP patients with platelets <10*10 9/L and bleeding symptoms requiring treatment, who were refractory to glucocorticoids and used thrombopoietic drugs. The bleeding score was calculated with reference to the Chinese guidelines for adult ITP. The patients were divided into three groups according to the medication used: rh-TPO group(rh-TPO 30000IU Qd), TPO-Ra group(Eltrombopag 25mg-75mg/d or Avatrombopag 2.5mg-7.5mg/d or Hetrombopagolamine 20mg-60mg/d), and rh-TPO+TPO-Ra group(combination of two drugs at the same dosage). The platelet count should be rechecked every 1-2 days during the treatment. Platelet transfusion and hemostatic drugs can be used as needed. According to the standardized and international criteria, and taking into account the characteristics of this study, platelet counts were classified as short-term Complete Response(sCR), short-term Response(sR), and short-term No Response (sNR), based on the highest value of platelet counts from the start of treatment to the time of hospital discharge, short-term Overall Response(sOR)=sCR+sR. The three groups were compared the effective time(defined as the time to first sCR/sR after treatment) , peak platelet count after treatment, time to peak platelet count after treatment and other short-term efficacy indicators.
Results
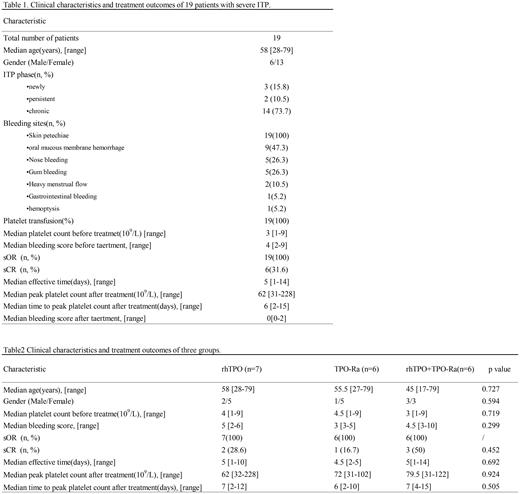
Nineteen patients were include in this study, with 68.4% (13/19) was female. The median age was 58 years [range 17-79]. 15.8%(3/19) were newly diagnosed with ITP, 10.5%(2/19) had persistent ITP, and 73.7%(14/19) had chronic ITP. All patients were treated with glucocorticoids prior to this treatment, but they had a poor response. The median platelet count was 3*10 9/L [range 1-9] and the median bleeding score was 4 [range 2-9] before treatment. The common bleeding sites were skin ecchymosis and oral mucous membrane hemorrhage in 100%(19/19)and 47.3%(9/19), respectively. Severe bleeding symptoms were the manifestation in 3 cases: including 2 heavy menstrual flow and 1 hemoptysis and gastrointestinal. 100%(19/19) achieved a sOR and 31.6%(6/19) achieved a sCR. The median bleeding score was 0[0-2] after treatment and none had active bleeding symptoms. Platelet transfusion and hemostatic drugs were administered to all patients. Further details are provided in Table 1.
Among 19 patients, 7(36.8%) used rh-TPO alone, 6(31.6%) TPO-Ra alone and 6(31.6%) used rh-TPO+TPO-Ra. There was no statistically significant difference in Clinical characteristics, including ages, gender, platelet counts and bleeding score among the three groups of patients before treatment (P=0.727, 0.594, 0.719, 0.299). In terms of treatment efficacy, we were unable to perform a statistical analysis of sOR rates because all three groups reached 100%. The sCR and the peak platelet count after treatment of rhTPO+TPO-Ra group was higher than the other two groups, 28.6%(2/7), 16.7%(1/6) and 50%(3/6) of patients achieved sCR respectively, the peak platelet counts after treatment in the three groups were 62*10 9/L, 72*10 9/L, 79.5*10 9/L respectively in this treatment, but there was no statistically significant difference (P=0.425,0.924). In addition, the effective time and time to peak platelet count after treatment of the three group are also no statistically significant difference(p=0.692,0.505). Further details are provided in Table 2.
Conclusion
This retrospective study suggests that the patients with severe ITP who were refractory to glucocorticoids, the use of rh-TPO and TPO-Ra may rapidly increase to safe ranges, but the combination is not necessary.
Disclosures
No relevant conflicts of interest to declare.