Introduction: Patients with liver injury have hemostatic defects including reduced ADAMTS13 (A disintegrin and metalloproteinase with thrombospondin type 1 motif, member 13). Severe deficiency of ADAMTS13 (ADMS13) activity (< 10%) is pathognomonic for thrombotic thrombocytopenic purpura (TTP), a rare thrombotic microangiopathy (TMA).
Differentiating TTP from severe liver injury is complex for multiple reasons including 1) low baseline ADMS13 2) concomitant coagulopathies complicating differentiation from disseminated intravascular coagulation (DIC) 3) ADMS13 activity (ADMS13:AC) assay interference (hyperbilirubinemia (>30mg/dL) can cause artifactual reduction of ADMS13:AC). Here we sought to characterize the clinical presentation, management, and outcomes of patients with liver injury presenting with thrombocytopenia (TCP), microangiopathic hemolytic anemia (MAHA) and low ADMS13:AC at our institution.
Methods: In this retrospective study, after IRB approval, electronic medical records (EMR) of institutional patients who had ADMS13:AC and inhibitor profile performed in our special coagulation laboratory between 2018 and July 17, 2023, were reviewed. Eligible patients had ADMS13:AC ≤20% were ≥ 18 years and had evidence of liver injury at time of ADMS13. Liver injury was defined as ALT or AST elevations greater than two times the upper level of normal within one month prior to ADMS13:AC testing, history of end stage liver disease or cirrhosis, or liver transplant with evidence of graft dysfunction. Details regarding clinical presentation, management and outcomes were extracted from the EMR. PLASMIC and ISTH DIC scores were retrospectively calculated.
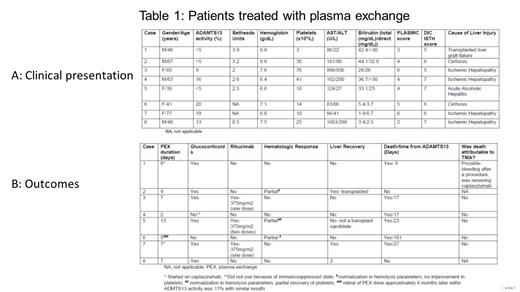
Results: 70 patients had at least one ADMS13:AC < 20% during the study period. 28/70 patients met liver injury inclusion criteria and 20/28 had TCP and MAHA. Of those 20 patients, median age at initial ADMS13:AC was 56.5 years (29-85). Most patients (n=14) had ADMS13:AC of 10-20%. ADMS13:AC was < 5% and 5-10% in 3 patients each. Eleven patients had a positive inhibitor with a median Bethesda titer of 1.85 BU (0.5-3.9). Etiology of liver included: ischemic hepatopathy (n=8), liver graft failure (n=4), liver metastasis (n=3), cirrhosis (n=2), alcoholic hepatitis (n=1), unknown (n=2).
Median hemoglobin and platelet (plt) count at time of ADMS13 was 7 g/dL (6.4-13.2) and 30 x10 9/L (3-98), respectively. 7/20 patients had a PLASMIC score of ≥5; PLASMIC score was ≥5, in 2/6 patients with ADMS13:AC <10%. 16/18 patients had an ISTH DIC score ≥5. 18/20 patients had a creatinine > 2 mg/dL or were receiving renal replacement therapy the time of ADMS13: AC. 7/20 patients had total or direct bilirubin of >30mg/dL.
Eight/20 patients were treated with plasma exchange (PEX) for a median duration of 7 days (2-13). 66.7% of pts with ADMS13:AC <10% received PEX. Glucocorticoids and Rituximab were used with the intent to treat TTP in 7 and 3 patients, respectively. Caplacizumab was used in 2 patients. 3/8 (37.5%) patients receiving PEX demonstrated normalization of MAHA. One of these patients demonstrated improvement but not normalization of plts (Table 1B, case 5). All patients had recurrence of hematologic abnormalities after PEX was stopped. One patient was treated with plasma infusion with stabilization in plt count. There were 13 and 15 deaths within 1 and 6 months of first ADMTS13:AC, respectively. One death was potentially attributable to management of TTP (Table 1B, case 1). There was no difference in time to death or mortality with the use of PEX. Repeat ADMS13:AC remote from PEX, TCP and MAHA was available for 1/5 surviving patients. This patient (Table1, case 2) had normalization of ADMS:AC after undergoing liver transplant.
Conclusion: The differential diagnosis of TCP and MAHA in patients with liver injury includes hepatic dysfunction, DIC and TMA. In the current cohort, 89% of evaluable patients met criteria for overt DIC per ISTH criteria. Due to a low ADMTS13:AC, 40% of patients underwent a trial of PEX with 37.5% demonstrating improvement in MAHA that was not sustained upon discontinuation of PEX due to persistent liver dysfunction. Six-month mortality was 75% and use of PEX did not affect mortality. Given the high mortality, further studies evaluating which patients with TMA and liver injury are more likely to benefit from therapies typically used to treat TTP are necessary.
Disclosures
Sridharan:Sanofi: Consultancy. Pruthi:CSL Behring: Consultancy, Honoraria; Instrumentation Laboratories (Werfen): Consultancy, Honoraria; Bayer Healthcare AG: Consultancy, Honoraria; Genentech Inc.: Consultancy, Honoraria; HEMA biologics: Consultancy, Honoraria.