Introduction: Acute lymphoblastic leukemia (ALL) is the predominant type of leukemia diagnosed in children and accounts for approximately 20% of all cases of acute leukemia in adults. In pediatric cases, ALL generally exhibits a favorable prognosis and outcome. Unfortunately, this optimistic scenario does not extend to adults, as the majority of deaths related to ALL occur in this age group. The outcomes observed in children with ALL are linked to the favorable cytogenetic profile of their leukemia. However, as individuals age, the cytogenetic profile progressively shifts towards high-risk groups. Furthermore, several epidemiologic studies have identified ethnicity, specifically Hispanic and African American backgrounds, as independent factors associated with worse outcomes. The factors contributing to these outcomes are diverse and include limited healthcare access, insurance coverage, immigration status, treatment adherence, socioeconomic status, and timeliness of treatment initiation, among others. Additionally, individuals of Hispanic ethnicity are more prone to complex cytogenetics and Central Nervous System involvement, both of which are commonly associated with a poor prognosis. Our study aimed to assess the differences in treatment outcomes among adults diagnosed with ALL by conducting a specific comparison between non-Hispanic and Hispanic individuals.
Methods: In this retrospective observational study, we collected data from the electronic medical records (EMR) of patients aged 18 years and older who received a diagnosis of Acute Lymphoblastic Leukemia between February 1, 2011, and February 28, 2020 at Ascension Seton Hospitals in Texas. The collected data included sociodemographic factors such as gender, ethnicity, and age at diagnosis, as well as clinical characteristics such as cytogenetics, immunophenotype, treatment, and overall survival. Bivariate and multivariate analyses were conducted using a chi-squared test. Statistical significance was defined as a P-value less than 0.05.
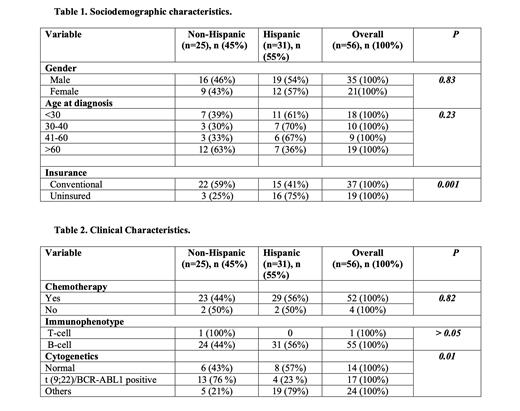
Results: A total of 56 patients with ALL were identified, with 45% being non-Hispanic and 55% being Hispanic. The incidence of ALL did not show significant variation based on gender or age, but it exhibited a significant difference depending on insurance status. The analysis revealed that Hispanic patients had a significantly higher likelihood of lacking insurance coverage (75%) compared to non-Hispanic patients (25%), with a statistically significant p-value of 0.001. With the exception of one non-Hispanic patient diagnosed with T-cell ALL, almost all participants in the study had B-cell ALL. Among the patients who received chemotherapy, 44% were non-Hispanic, while 56% were Hispanic. Among patients with t(9;22)/BCR-ABL1 positive ALL, non-Hispanics represented 76% and Hispanics represented 23%. Other cytogenetic abnormalities, including CRLF2-IGH fusion, IgH rearrangement, CRLF2 rearrangement, PBX1/TCF3 fusion, t(1;19) with PBX1/TCF3 fusion, ETV6 deletion, near haploidy, and 9p deletion, were more prevalent in Hispanic patients (79%) compared to non-Hispanic patients (21%). The overall survival rates at 1 year were 64% for non-Hispanic patients and 67.7% for Hispanic patients. However, at 3 years, the overall survival rates decreased to 32% for non-Hispanic patients and 25.8% for Hispanic patients.
Conclusions: Our study provides important insights into the demographic and clinical characteristics of patients with ALL and highlights notable disparities between non-Hispanic and Hispanic patients. A higher proportion of Hispanic patients lacked any form of health insurance coverage at the time of diagnosis. Interestingly, the incidence of Philadelphia-positive ALL was found to be higher among non-Hispanic patients, whereas other cytogenetic abnormalities were more prevalent among Hispanic patients. Additionally, Hispanic patients experienced lower rates of overall survival at 3 years, suggesting potential disparities in outcomes. The differences observed between Hispanic and non-Hispanic patients highlight the necessity for additional investigation and tailored interventions to address the specific challenges faced by Hispanic patients, including access to healthcare, insurance coverage, and the prevalence of unfavorable cytogenetic abnormalities.
Disclosures
No relevant conflicts of interest to declare.