Introduction
Thrombosis, both arterial and venous, is a major source of morbidity and mortality in patients with myeloproliferative neoplasms (MPNs). Thrombosis can be the initial presentation of MPN and sometimes can predate its diagnosis. Most MPN-related thrombosis occurs on usual sites such as the cerebral and coronary arteries, and lower limbs deep venous thrombosis and pulmonary embolism. Rare thromboses can also occur with MPN, such as splanchnic and cerebral dural vein thromboses, with the former having a stronger correlation. Stroke in young people (under 50) and venous thrombosis at unusual sites (cerebral, splanchnic, renal and upper limbs) represent special scenarios for which workup includes exploring unusual etiologies, including inherited and acquired hypercoagulable states.
JAK2 mutation is invariably present in polycythemia vera (PV), occurs in a significant proportion of other classical MPNs, and is directly associated with risk of thrombosis due to associated leukocytosis, platelet activation, and altered vascular endothelial function. JAK2-mutated MPNs are associated with higher thrombosis risk compared to JAK2 unmutated MPNs, and greater allele burden corresponds to greater risk.
The association of JAK2 mutation with hepatic and splanchnic vein thrombosis is well established. There are evidence-based guidelines for testing in idiopathic splanchnic vein thrombosis; however, its association with other unusual site thrombosis is unclear. Clinicians may request JAK2 mutation testing in individuals with unprovoked VTE and VTE at unusual sites to uncover the underlying etiology. This is despite a low diagnostic yield, particularly in people with normal CBC. Cerebral sinus thrombosis, for example, occurs in 1% of MPNs, and an underlying MPN accounts for only 3.8% of CVT. Most documented MPNs presenting with thrombosis had abnormal CBC at presentation, either thrombocytosis or erythrocytosis.
The aim of this analysis is to explore whether JAK2 mutation without overt MPN contributes to the unusual site venous thrombosis and stroke in young people in a high altitude population.
Method:
We collected lab records for all JAK2 requests made over three years (2020-2022) in two referral hospitals serving a population residing at an altitude of 2,270-3,000 meters above sea level. Requests that listed thrombosis as an indication were analyzed, and labs and imaging related to the corresponding requests were reviewed.
Results:
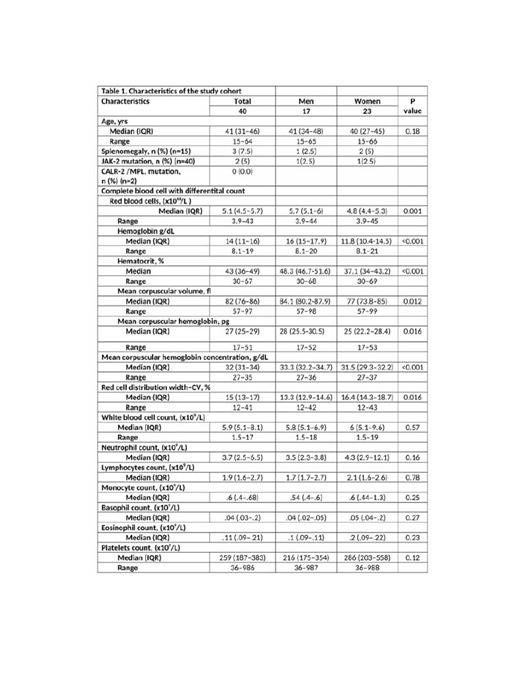
Among 208 JAK2 tests, 40 (19.2%) were requested during the evaluation of thrombotic events. Patients were relatively young, with a median age of 41, and the gender breakdown was 17 (42.7%) males and 23 females. About half (23, 57.5%) of the cohort had normal CBC. Those with abnormal CBC at presentation included 3 patients with leukocytosis, 10 with thrombocytosis, and 10 with erythrocytosis.
Among males, 2 had an ischemic stroke, 5 had cerebral sinus thrombosis, 5 had splanchnic vein thrombosis, 4 had unprovoked DVT/PEs, and 1 had renal vein thrombosis. Among females, 4 experienced ischemic strokes, 3 had cerebral venous thrombosis, 10 had splanchnic vein thrombosis, 5 had unprovoked DVT/PEs, and 2 had renal vein thrombosis. Only 2 patients (5%) were positive for JAK2 mutations: a 17-year-old boy who presented with portal vein thrombosis and was diagnosed with polycythemia vera and a 31-year-old lady who presented with hepatic vein thrombosis and normal CBC.
Conclusion:
JAK2 mutation was rare in our high-altitude cohort with unprovoked DVT/PE/thrombosis at unusual sites. Outside the splanchnic venous system and with normal CBC, the diagnostic yield of JAK2 mutation testing is low. Hence, such testing might not be indicated.
Disclosures
No relevant conflicts of interest to declare.