Introduction: Monoclonal gammopathy of undetermined significance (MGUS) is clinically defined with a serum monoclonal immunoglobulin of less than 3 g/dL and the presence of less than 10% of plasma cells in the bone marrow, in the absence of any end-organ damage that is typically seen in patients with multiple myeloma. The incidence of MGUS mostly involves the elderly, with a median age estimated at 70 years. While some studies have linked MGUS with a hypercoagulable state, there are no large studies investigating the impact and outcomes of MGUS in the elderly with pulmonary embolism(PE). We thus propose a national analysis to investigate.
Methods: Our retrospective study via the National Inpatient Sample (NIS) focused on adults admitted with a primary diagnosis of Acute Pulmonary Embolism. We excluded all cases of ages <70 years and >90 years. Patient characteristics in acute PE cases with and without MGUS such as age, sex, race, and presence of various comorbidities such as diabetes, hypertension, obesity, among many, were explored via Chi-Square tests, t-tests, and Mann-Whitney U tests as appropriate. Differences in outcomes for PE in MGUS and non-MGUS patients were estimated via logistic regression models on SPSS 29.0. A p-value of <0.05 was considered as statistically significant. To comply with the database provider's (HCUP) guidelines, we did not report values <11.
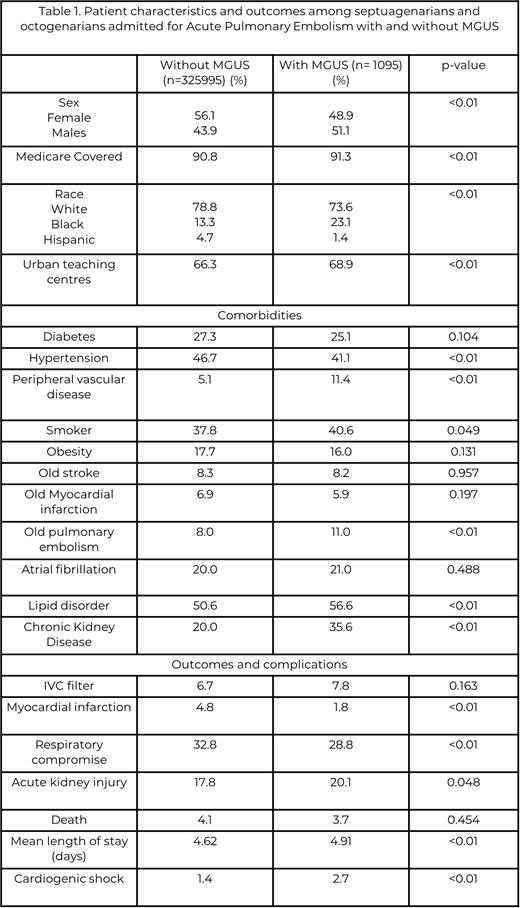
Results: Among the 327090 septuagenarians and octogenarians admitted primarily for acute PE in our study, there were 1095 (0.3%) patients with a diagnosis for MGUS that also reported a higher mean Charlson Comorbidity Index (CCI) score (4.26 vs. 2.90, p<0.01) (Table 1). While 51.1% of MGUS cases with acute PE were males, the non-MGUS group mainly consisted of females (56.1%, p<0.01). Medicare covered 91.3% and 90.8% of all MGUS and non-MGUS cases in our study, and 68.9% and 66.3% of all admissions involved Urban-teaching centers, respectively. Around 11.0% of MGUS cases also had a history of prior pulmonary embolism, while it was 8.0% in the non-MGUS cohort (p<0.01). The MGUS cohort also showed a lower prevalence of hypertension (41.1% vs.46.7%, p<0.01) while having a higher prevalence of peripheral vascular disease (11.4% vs. 5.1%, p<0.01), smoking status (40.6% vs. 37.8%, p=0.049), lipid disorders (56.6% vs. 50.6%, p<0.01), and chronic kidney disease (35.6% vs. 20.0%, p<0.01) than the non-MGUS group.
MGUS patients showed lower odds of experiencing in-patient events such as myocardial infarction (aOR 0.345, 95% CI 0.221-0.538, p<0.01), acute kidney injury (aOR 0.843, 95% CI 0.719-0.990, p=0.037), and respiratory compromise (aOR 0.749, 95% CI 0.652-0.860, p<0.01). While a higher odds of cardiogenic shock (aOR 1.903, 95% CI 1.316-2.753, p<0.01) was also noted, patients with and without MGUS had no differences related to in-hospital mortality (aOR0.721, 95% CI 0.513-1.013, p=0.060) or the need for IVC filters (aOR 1.156, 95% CI 0.924-1.446, p=0.206). MGUS patients also experienced a longer stay (mean length of stay 4.91 vs. 4.62 days, p<0.01).
Conclusion: This nationwide data analysis suggests a higher prevalence of a history of previous PE in MGUS cases admitted for PE than those without MGUS. Furthermore, while odds of events involving in-patient myocardial infarction, acute kidney injury, or respiratory compromise in MGUS patients were lower, they had a higher risk of cardiogenic shock. It is thus vital for physicians to be on the watch-out of such complications and provide adequate testing and care in a timely manner to improve their prognosis and outcomes.
Disclosures
No relevant conflicts of interest to declare.