Introduction
Patients undergoing anti-CD19 chimeric antigen receptor T cell (CAR T) therapy for the treatment of aggressive B-cell non-Hodgkin lymphomas (B-NHL) can expect a complete response rate of merely 43-68%. Insubstantial clinical responses to CAR T therapy and a small window of survival for patients facing relapsed/refractory (R/R) disease highlights the critical need for improvement of CAR T therapy in aggressive B-NHL cases. Recent findings suggest that enriching for a CD8 + T Stem Cell Memory (T SCM) population within adoptive cell therapies translates to enhanced antitumor function and persistence in vivo, and thus produces favorable clinical outcomes. T SCM cells display heightened self-renewal, low mitochondrial membrane potential (∆Ψm), and are metabolically dependent upon oxidative phosphorylation (OXPHOS) and fatty acid oxidation (FAO). Selection of CD8 + T SCM subsets is therefore necessary to ensure a robust antitumor response. Previously, we revealed synergy between the Bcl-2 inhibitor, Venetoclax, and CAR T cells in the context of B-NHL. Venetoclax exposure increased CD8 + T SCM cell frequency, decreased ∆Ψm, reduced T Regulatory (T REG) cell frequency, and bolstered effector cytokine production. Though the role of Bcl-2 inhibition within B-NHLs is well characterized (FDA-approved for frontline and relapsed/refractory chronic lymphocytic leukemia [CLL] treatment), further investigation regarding the impact of Venetoclax on the patient T cell compartment is needed. In this study, we demonstrate a role for Venetoclax as a qualitative enhancer of bulk CAR T cell product using both healthy-donor and B-NHL patient-derived T cells, and implicate modulation of mitochondrial pathways as a likely mechanism of action.
Methods
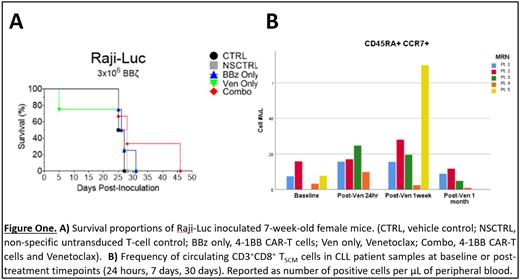
Whole peripheral blood mononuclear cells were collected from consenting healthy human donors or CLL patients undergoing ramp-up with Venetoclax (BDR 164122) at Roswell Park Comprehensive Cancer Center, and activated with αCD3/αCD28. CLL samples were collected at baseline, 1 day, 7 days, and 1-month timepoints. Transduction was performed with lentiviral vectors encoding CD28 or 4-1BB-based α-CD19 CAR constructs 24 hours post-activation. Transduced cells were cultured in RPMI with hIL-2 and hIL-7. In vivo studies were performed on 7-week-old SCID mice using Raji-Luc, Rec-1, and U2932. Venetoclax was given daily [100mg/kg] via oral gavage. CAR T cells were delivered by single infusion via tail-vein injection at a dose of either 1x10 6 or 3x10 6 cells total.Mice were imaged via IVIS spectrum. Western blot was performed on stimulated untransduced T cells or CAR T cells exposed to Venetoclax. Total protein was quantified, and membranes were probed for apoptotic and mitochondrial protein expression. Patient sample immunophenotyping was performed on CLL patient samples using panels interrogating memory differentiation, exhaustion, and T REG populations.
Results
Consistent with our hypothesis, a significant increase in mitochondrial proteins associated with FAO and OXPHOS - ACC, PDH, and AMPKα - was observed in exposed CAR T cells, as well increased expression of transcription factor FOXO1 - an essential driver of CD8 + memory differentiation. Voltage-dependent anion channel (VDAC) expression increased, suggesting heightened efflux of respiratory substrates into the tricarboxylic acid cycle. Hexokinase-I, a critical glycolytic enzyme, was significantly downregulated. We next investigated our combination therapy in vivo and observed extended survival outcome by 15 days. Further in vivo studies investigating preclinical models of mantle cell lymphoma and activated B-cell diffuse large B-cell lymphoma are currently ongoing. Within our CLL patient samples, 24-hour and 7-day timepoints reflected a favorable population increase in CD8 + T SCM cells as compared to baseline samples, and marginally restored CD8 + T cell frequencies.
Conclusion
Metabolic properties guide T cell memory differentiation and fitness. There exists potential to manipulate this mechanism and select the most metabolically fit T cell population for adoptive cell therapies. In addition to answering fundamental questions of CAR T cell biology, the combination of Venetoclax and CAR T cell therapy may provide a solution to the observed clinical gap, in which CAR T therapy as a single agent does not afford favorable response rates in the context of aggressive and R/R B-NHLs.
OffLabel Disclosure:
Hernandez-Ilizaliturri:ADC Therapeutics: Consultancy; Dava Oncology: Consultancy; Novartis: Consultancy; Amgen: Consultancy; Collectar: Consultancy; Gilead: Consultancy; Kite: Consultancy; Incyte/Morphosys: Consultancy; BMS: Consultancy; AbbVie: Consultancy; Epizyme: Consultancy; BioGene: Consultancy.
Bcl-2 inhibitor Venetoclax (ABT-199) is a small molecule inhibitor which is FDA-approved for the treatment of chronic lymphocytic leukemia and small lymphocytic leukemia. In this study, Venetoclax is repurposed in the context of B-cell non-Hodgkin lymphoma to improve anti-CD19 CAR-T cell fitness and quality.