Introduction
Allogeneic hematopoietic cell transplantation (allo-HCT) is a curative treatment for patients with hematological malignancies. Steroid-refractory chronic GVHD (SR-cGVHD) remains the major cause of non-relapse mortality and life-threatening disease late after allo-HCT. Several groups reported that perturbation in the gut microbiome and impaired production of microbial metabolites such as short chain fatty acids (SFCAs) have involved in cGVHD pathogenesis and severity. Currently, there is no acceptable consensus and no standard second-line treatments for patients with SR-cGVHD. Our pilot study (NCT04622475) using fecal microbiota transplantation (FMT) from healthy donor to treat patients with SR-cGVHD provide a new insight into therapeutic strategies for SR-cGVHD. To investigated whether FMT improves the SR-cGVHD clinical outcome through SCFAs, the measurement of SCFAs concentration was performed in the plasma from SR-cGVHD patients after FMT. Here we report the preliminary results of this study.
Method
12 patients aged 16-60 years with SR-cGVHD after allo-HCT were enrolled. A total of 31 FMTs were performed via colonoscopy in 12 patients with SR-cGvHD over three consecutive months. FMT courses were repeated from the same donor. To characterize the impact of the FMT on the gut microbiota, stool samples and plasma from recipients were collected the day before FMT treatment and 4 weeks after each FMT treatment then carried out 16s rRNA sequencing and LC-MS. Complete response was defined as the complete resolution of GVHD manifestations in all organs. Partial response was defined as a decrease at least one stage in severity of GVHD or able to taper steroid dose. No response was defined as unable to taper steroid dose or need to increase or add immunosuppressor for controlling GVHD progression.
Result
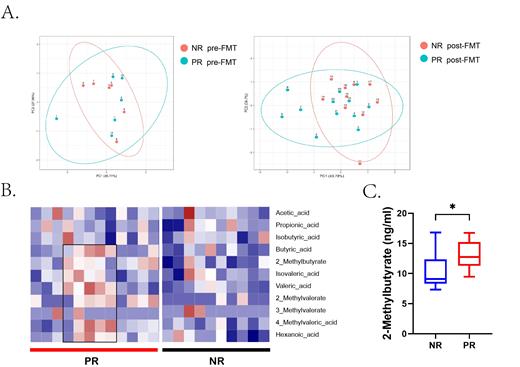
The circulating SCFAs levels of SR-cGVHD patients associated to FMT outcome (Figure A). After FMT, the concentrations of butyric acid, isovaleric acid, valeric acid, 4-Methylvaleric acid and hexanoic acid had a higher trend in the plasma of responders, but not in the non-responders (Figure B). Notably, 2-Methylbutyrate markedly increased in the plasma of responders after FMT, when compared to non-responder after FMT(Figure C).
Conclusion
The present study indicates that FMT improved SR-cGVHD patients by increasing the circulating SCFAs, particularly 2-Methylbutyrate levels. 2-Methylbutyrate might play a role in FMT therapy for SR-cGVHD.
Disclosures
No relevant conflicts of interest to declare.
Disclosures
No relevant conflicts of interest to declare.