Objective: This article primarily examines the clinical attributes of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in transplant recipients with thalassemia, offering significant insights into the treatment and care of this patient population.
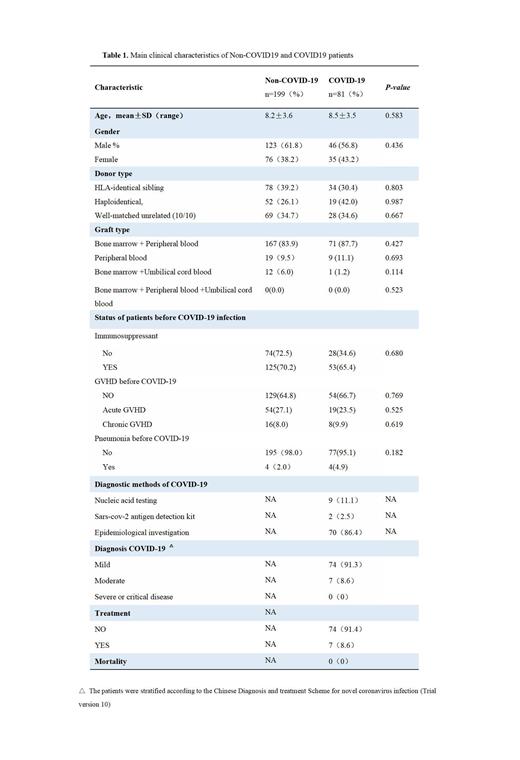
Method: The present study retrospectively analyzed the data of all thalassemia patients who underwent Hematopoietic stem cell transplantation (HSCT) at the First Affiliated Hospital of Guangxi Medical University between December 2019 and December 2022. A total of 280 patients were included, of which 81 had confirmed coronavirus disease 2019 (COVID-19). The study collected information on patient demographics, transplantation type and timing, graft-versus-host disease (GVHD), use of immunosuppressive agents, onset time and severity of COVID-19, and prognosis. Follow-up was conducted until March 31, 2023.Univariate analysis was performed using SPSS v25.0, and GraphPad Prism was used for the cumulative incidence comparisons.
Results: The median age was 3.6(2-19) years.The main type of thalassemia was β type (93.9%). Identical sibling donors accounted for 40%, haploidentical donors accounted for 25.4%, and identical unrelated donors accounted for 34.6% (10/10). The main source of hematopoietic stem cells was bone marrow combined with peripheral blood (85%).There were no significant differences in age, gender, diagnosis, donor type, graft type, use of immunosuppressive agents, GVHD, and pneumonia of pro-COVID-19 between infected patients and non-infected patients with SARS-CoV-2. Most of the patients were mild (74 cases, 91.3%) in terms of the severity of COVID-19 infection, only 8.6% of the moderate cases, and none severe and died. 74 cases were cured without drug treatment. Of the seven patients treated with medications, four were azvudine and three were nematasvir. The median number of days (IQR) of treatment for COVID-19 was 5(5) days. The cumulative incidence in the immunosuppressive group was higher than that in the non-immunosuppressive group over the same time frame. There was no significant difference in the final infection rate of COVID-19 among patients receiving transplantation in different years(2020,2021,2022), which was 24.7 26.8 36.5 ( p=0.368), respectively.
Conclusion:
The low infection rate and no severe cases may be due to scientific protection and timely medication. There are no special risk factors for COVID-19 infection in thalassemia patients after transplantation.
Disclosures
No relevant conflicts of interest to declare.