Objective: Patients with hematologic diseases are at a higher risk for Stenotrophomonas maltophilia(SM) bacteremia, which poses significant burden on morbidity and mortality. The aim of this study was to evaluate the early predictors of 28-day mortality in hematologic patients with SM bacteremia and to construct a reliable prediction model which can be used to identify patients at higher risk for mortality.
Methods: This retrospective analysis of 131 hospitalized patients diagnosed with SM bacteremia was conducted in a tertiary blood disease center in Tianjin, China, from January 2012 to June 2023. Univariate analysis and multivariate logistic regression analysis were used to identify prognostic risk factors and develop a prognostic mortality scoring system and internally validated by bootstrap method (resampling = 1000).
Results: The overall 28-day mortality rate in our study was 29.77% (39/131). The mean age was 45 (IQR 30.5-56.0) years and 70 individuals (53.44%) were diagnosed with myeloid malignancies. The existing condition severity-related scores did not perform well in predicting 28-day mortality for the patients in our population (AUROC values: SOFA: 0.842; ECOG: 0.831; APACHE Ⅱ: 0.709; SAPS Ⅱ: 0.675; aCCI: 0.654; Pitt score: 0.629).
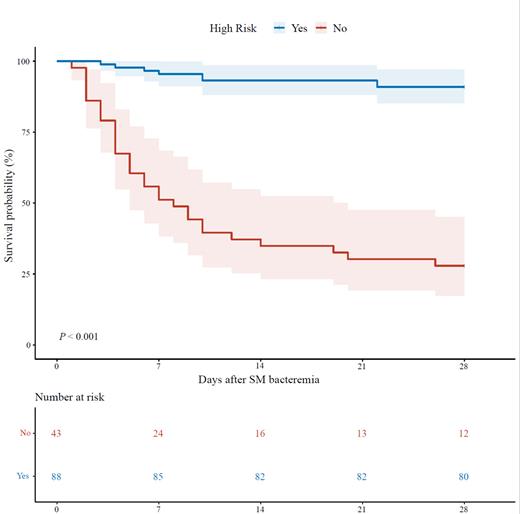
Through univariate and multivariate analysis, we identified four independent risk factors associated with 28-day mortality: SOFA score (OR = 3.67, 95% CI 1.99-6.78, P < 0.001; score = corresponding SOFA score), age ≥ 60 years (OR = 6.95, 95% CI 1.44-33.55, P = 0.0158; score = 2), bloody sputum or hemoptysis (OR = 5.32, 95% CI 1.08-26.29, P = 0.0402; score = 2) and neutropenia duration ≥ 25 days (OR = 3.92, 95% CI 1.01-15.26, P = 0.0487; score = 1). These factors were used to develop a prognostic scoring model, which yielded good discrimination (AUC = 0.889, 95% CI: 0.829-0.949) and calibration (Hosmer-Lemeshow goodness-of-fit test P = 0.998), with similar performance in the internal bootstrap validation (AUC = 0.888). Furthermore, all patients were divided into the high-risk group (≥ 7 points) and the low-risk group (< 7 points) based on the model and compared using Kaplan-Meier curves and log-rank tests. Additionally, we founded that the use of trimethoprim-sulfamethoxazole (TMP/SMX) after infection was associated with a better prognosis ( P = 0.012).
Conclusions: The prediction model, utilizing SOFA score, age, bloody sputum or hemoptysis and neutropenia duration, proves to be an effective tool for early identification of hematologic patients with SM bacteremia at high risk of mortality.
Disclosures
No relevant conflicts of interest to declare.