Background: Coagulation factor XII (FXII) has drawn significant attention as a potential drug target due to the observation that severe congenital deficiency in FXII is not associated with bleeding, while deletion or inhibition of FXII in pre-clinical models consistently protects against thrombosis. However, the contribution of FXII to thrombosis in humans remains controversial, with early reports suggesting that FXII deficiency may even be associated with an increased risk of venous thromboembolism (VTE). Meanwhile, epidemiologic studies of FXII deficiency have yielded conflicting results and are fraught with methodological challenges in part because FXII-deficient patients have no known phenotype and do not typically present to medical attention. To overcome these limitations, we performed the first large-scale analysis of differential thrombotic risk associated with germline loss of function in the gene encoding FXII ( F12) across over 400,000 individuals.
Aims: To determine the impact of rare F12 loss-of-function variants on the risk of VTE in a large-scale whole exome sequencing dataset.
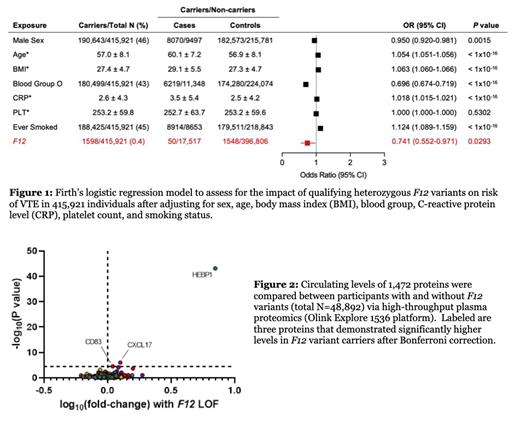
Methods: The UK Biobank (UKBB) is a population-scale registry dataset containing paired clinical and genomics data for nearly 500,000 individuals. We identified individuals in the UKBB with rare (MAF <1%) variants in F12 that were predicted in silico to result in altered protein function. Qualifying variants included missense variants with an in silico functional impact score of ≥0.9 and high-confidence loss-of-function (HCLOF) variants such as frameshift, nonsense, and essential splice site mutations. We used Firth's logistic regression to assess the association between qualifying F12 variants in a single-gene collapsing analysis and the risk of VTE after adjusting for age, sex, and ancestry as well as several known contributory factors. Differences in the levels of 1,472 plasma proteins between carriers and non-carriers of qualifying F12 variants were evaluated in a subset of 48,892 UKBB participants using the Olink Explore 1536 proteomics platform.
Results: Data from 415,921 UKBB participants were included in our analysis. In total, 1,598 individuals carried qualifying variants in F12, of which 99.8% were heterozygous. The presence of rare, function-altering variants in F12 was significantly associated with protection against VTE (OR=0.74, 95% CI: 0.55-0.97, P=0.029) ( Figure 1). This finding remained unchanged when we restricted the analysis to HCLOF variants (OR=0.74, 95% CI: 0.55-0.97, P=0.031). Further, we replicated several known risk factors for VTE, including female sex (P=0.0015), older age (P<1 x 10 -16), higher BMI (P<1 x 10 -16), non-O blood group (P<1 x 10 -16), higher CRP (P<1 x 10 -16), and a history of smoking (P<1 x 10 -16), suggesting that clinical annotation for the dataset is reliable. As expected, the presence of F12 variants was not associated with increased risk of hemorrhage (OR=0.90, P=0.44). Because FXII is also involved in pathways of innate immunity, we interrogated the relationship between carriage of rare F12 variants and sepsis and found no increased risk (OR=0.95, P=0.73). Next, we compared the circulating plasma levels of 1,472 proteins between participants with and without qualifying F12 variants ( Figure 2). We determined that plasma concentrations of three proteins are significantly elevated in participants with a variant F12 allele. Of these, heme binding protein 1 (HEBP1) levels demonstrated the most striking difference (fold-change=7.08, P=1.439 x 10 -43). However, germline loss-of-function variants in the HEBP1 gene are not associated with decreased risk of VTE (OR=1.109, P=0.88), suggesting that HEPB1 levels are regulated by FXII and do not directly influence VTE risk.
Conclusions: Operating at the level of germline genetics, our data are the first to demonstrate that FXII loss-of-function is protective against VTE in humans. Because F12 variant carriers in the UKBB dataset predominantly possess only a single defective allele, it is possible that larger effect sizes would be observed among homozygous or compound heterozygous individuals. Additionally, F12 loss-of-function does not appear to increase the risk of hemorrhage or severe infection. Our findings suggest that therapeutic blockade of FXII in humans is likely to be safe and effective.
Disclosures
Grover:CSL Behring: Research Funding. Ellinor:Novartis: Consultancy; Bayer AG: Consultancy, Research Funding. Bendapudi:Alexion Pharmaceuticals: Consultancy; Takeda Pharmaceuticals: Consultancy.