In this issue of Blood, Tsyplenkova et al identify a role of the non–iron-loaded transport protein apotransferrin (apo-Tf) in enhancing dietary iron absorption.1
Dietary iron malabsorption is frequently observed in a variety of intestinal diseases, such as celiac disease, inflammatory bowel disease, or Helicobacter pylori infections, that may culminate in iron deficiency anemia.2 The pathophysiological mechanisms of dysfunctional iron absorption in these conditions are not completely understood, and often iron supplementation is insufficient. At present, the primary recognized iron absorption regulatory mechanisms focus on limiting the export of absorbed dietary iron from duodenal enterocytes into the bloodstream. These mechanisms include the regulated expression of the iron exporter ferroportin, and the induction of the liver-produced hormone hepcidin, which limits iron uptake by promoting degradation of ferroportin.3
Transferrin, the primary iron transport protein in the bloodstream, binds iron released by enterocytes via ferroportin.4 This process is facilitated by ferroxidases, such as hephaestin (see figure). Transferrin then delivers this iron to erythroblasts in the bone marrow or other cells.5 Empty transferrin devoid of iron is called apo-Tf, whereas iron-loaded transferrin is named holo-Tf. Although high levels of holo-Tf induce the expression of hepcidin and limit iron absorption, apo-Tf was not considered to have a regulatory role in iron uptake until recently. Such a controlling role is now supported by a new study of Tsyplenkova et al.
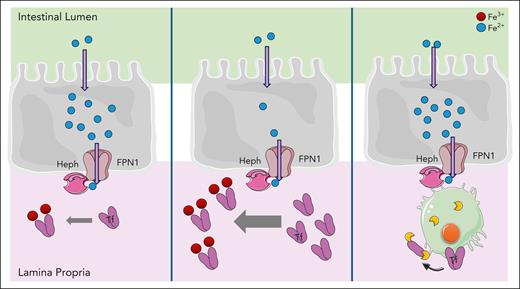
A model for regulation of dietary iron absorption by transferrin (Tf) and macrophages in the duodenum. The presence of apo-Tf allows the efflux from enterocytes via ferroportin (FPN1) and the ferroxidase hephaestin (Heph), which oxidizes Fe2+ to Fe3+ to allow scavenging on Tf (left panel). When more apo-Tf is available, for example by injection of apo-Tf, a higher iron efflux through FPN1 is stimulated by providing more acceptor molecules, shifting the equilibrium (middle panel). Macrophages in the lamina propria can degrade Tf via the action of proteases and thereby reduce iron efflux from enterocytes (right panel).
A model for regulation of dietary iron absorption by transferrin (Tf) and macrophages in the duodenum. The presence of apo-Tf allows the efflux from enterocytes via ferroportin (FPN1) and the ferroxidase hephaestin (Heph), which oxidizes Fe2+ to Fe3+ to allow scavenging on Tf (left panel). When more apo-Tf is available, for example by injection of apo-Tf, a higher iron efflux through FPN1 is stimulated by providing more acceptor molecules, shifting the equilibrium (middle panel). Macrophages in the lamina propria can degrade Tf via the action of proteases and thereby reduce iron efflux from enterocytes (right panel).
Any iron that is not sequestered by transferrin or other traditional iron-binding proteins in the blood is called non–transferrin-bound iron (NTBI). NTBI is usually detectable on feeding mice a high-iron diet, potentially because the newly absorbed iron can no longer be scavenged by endogenous transferrin when it is fully saturated. Hence, Tsyplenkova et al reasoned that infusion of free apo-Tf should increase total iron-binding capacity and should be able to prevent the formation of NTBI. Hence, they injected apo-Tf at the time when mice were switched from a low- to a high-iron diet and compared them with mice on a high-iron diet only. Six hours after apo-Tf injection, transferrin-bound iron (TBI) was increased 3-fold in the serum, whereas, surprisingly, NTBI was not reduced but rather enhanced. Moreover, expression of Hamp, the gene encoding for hepcidin, was significantly induced in the liver. These data suggested that the injection of apo-Tf directly stimulated dietary iron absorption (see figure).
To confirm these findings, Tsyplenkova et al explored more iron states in their mouse model. Mice previously fed an iron-deficient diet were injected with apo-Tf and compared with those left untreated with or without switching to a high-iron diet. Again, when high iron was provided in the diet, apo-Tf strongly increased TBI and NTBI. Apo-Tf also prevented iron accumulation in the duodenal enterocytes after high iron feeding, suggesting enhanced iron efflux into the serum. Apo-Tf injection under low dietary iron conditions did not strongly increase serum TBI nor NTBI levels but reduced Tf saturation and increased total iron-binding capacity, as expected. This supported the conclusion that apo-Tf increases dietary iron uptake but does not induce iron mobilization from other tissues. Interestingly, the increase in iron absorption was also seen, although reduced, in mice kept on a standard diet and challenged with a high-iron diet together with apo-Tf. Overall, these data implied that injected apo-Tf can enter the duodenum and directly stimulate iron efflux from ferroportin potentially by shifting the thermodynamic equilibrium by providing more iron acceptor molecules to ferroportin.
To confirm that injected transferrin reached the duodenum, the authors infused apo-Tf spiked with a fluorescently labeled transferrin. Indeed, the labeled transferrin could be readily detected in the duodenum, but also in the liver and spleen. Remarkably, the transferrin in the duodenum localized to macrophages in the crypt areas of the lamina propria, whereas in the liver and spleen, the transferrin localized to nonmacrophage cells. Macrophages are known to control various aspects of iron metabolism in the liver, spleen, and bone marrow,6 but only recently emerged to regulate iron metabolism in the duodenum.
In a recent study also in Blood, it was shown that macrophages in the villous lamina propria of the duodenum can regulate dietary iron absorption by locally degrading transferrin via proteases and, thus, potentially limiting iron efflux from the enterocytes (see figure).7 These data suggested that the local levels of transferrin are actively controlled, and regulated transferrin expression was also found during the prandial process or during Citrobacter infection. The current report by Tsyplenkova et al supports and extends the previous results by showing that serum transferrin can reach the crypt area of the lamina propria and specifically interact there with macrophages. Although the exact nature of the labeled transferrin in their studies and its interaction with macrophages are unknown, it may not include transferrin receptors but may involve endocytosis.8
In addition, other questions remain unanswered: Is the presence of transferrin in the duodenum correlated with the iron status in anemia? Is this also associated with macrophage activation in such diseases? Does injection of apo-Tf influence macrophage activation, or does interference with macrophage activation influence the action of apo-Tf? May apo-Tf also regulate iron uptake via other nonduodenal mechanisms? Finally, the study by Tsyplenkova et al may also have therapeutic potential: does injection of apo-Tf enhance iron absorption in anemia, especially when given together with dietary iron supplementation?
Previously, apo-Tf was thought to simply transport iron but not to influence how much iron enters the bloodstream. The new data suggest that apo-Tf may not only be seen as iron transporter, but also as a novel iron regulation checkpoint via its availability in the duodenum in general.
Conflict-of-interest disclosure: The author declares no competing financial interests.