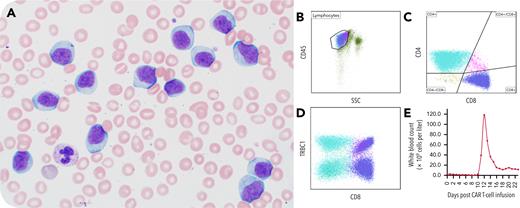
A 66-year-old man with relapsed multiple myeloma presented with rapid onset leukocytosis 12 days postinfusion of ciltacabtagene autoleucel, a chimeric antigen receptor (CAR) T-cell therapy. His white blood cell count was 118.2 × 109 cells per liter with absolute lymphocytosis (97% by manual differential). A peripheral smear showed numerous atypical lymphocytes of intermediate size with pale blue cytoplasm, irregular nuclei, mature chromatin, and variably-prominent nucleoli (panel A, Wright-Giemsa stain, ×60 objective). No circulating plasma cells were seen. Flow cytometry of the peripheral blood detected CD3-positive T cells that were a mixture of CD4-positive and CD8-positive T cells (CD4:CD8 ratio, 0.83) with an absence of B cells (panels B,C). T cells showed a polytypic pattern of T-cell receptor beta constant 1 (TRBC1) expression, supporting a reactive T-cell expansion (panel D). The patient was treated with dexamethasone 10 mg twice a day until his white blood cell count was <30 × 109 cells per liter, and then dexamethasone was tapered. The prominent lymphocytosis resolved within weeks (panel E). Three months after CAR T-cell therapy, the patient developed immune effector cell–associated neurotoxicity syndrome, for which he received treatment, and had no evidence of recurrent plasma cell neoplasm.
This case demonstrates the profound lymphocytosis that can be seen following CAR T-cell therapy and emphasizes the spectrum of atypical lymphocytes that can be seen on peripheral smears.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.